Knock Knees (Genu Valgum): Causes, Symptoms, Diagnosis, and Treatment
Medically reviewed by Dr. Neelabh, MS (Orthopedics) Educational information only—always consult a qualified Orthopedic specialist for diagnosis and treatment.
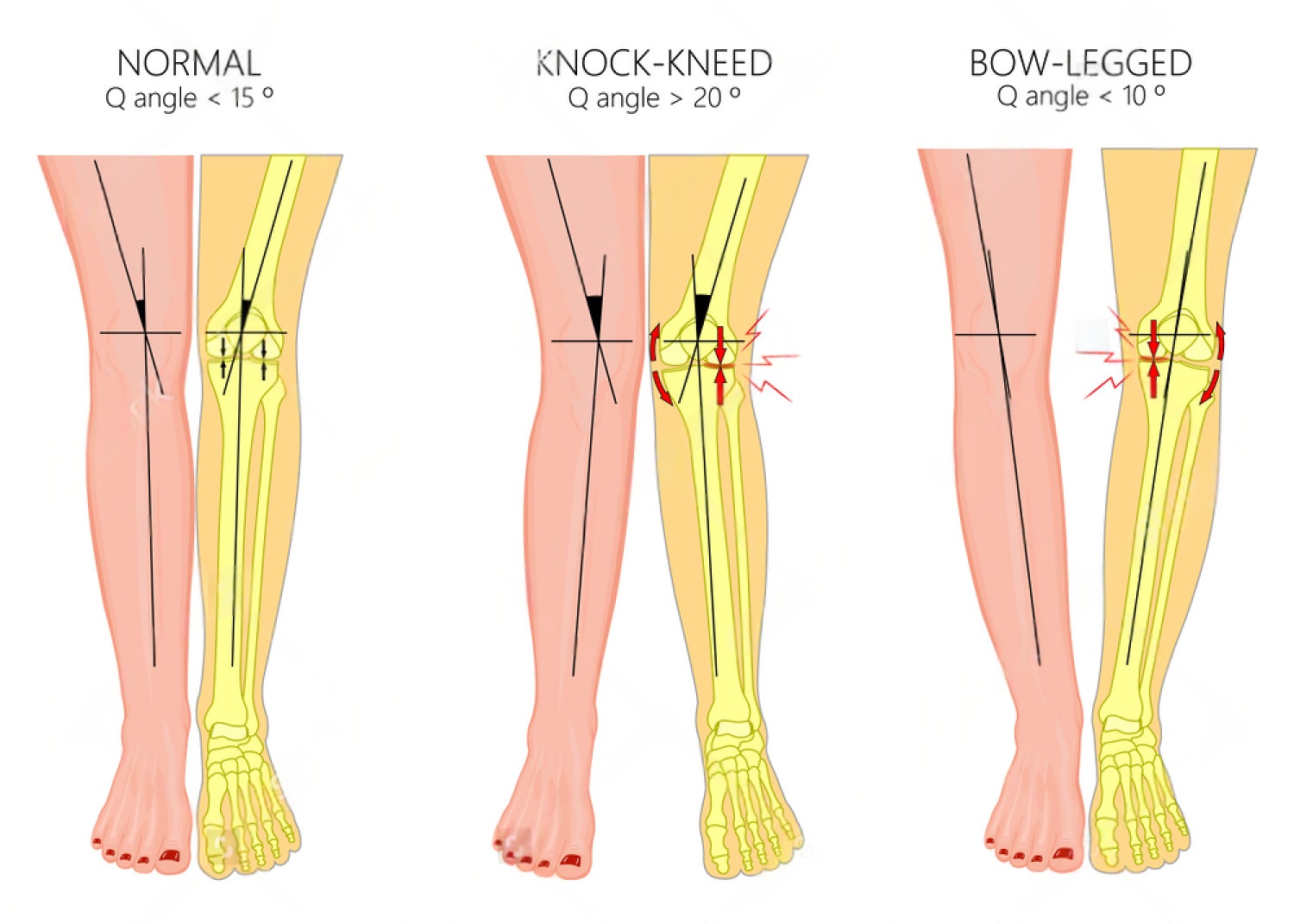
Knock knees (genu valgum) describes inward angling of the knees so they touch or nearly touch while the ankles stay apart. It is a normal phase of growth in many children and usually corrects on its own. When valgus is severe, asymmetric, painful, or persists, an expert evaluation helps determine the cause and best treatment.
On this page
Normal Development: What’s Expected by Age
A child’s leg alignment naturally changes as they grow. Understanding these phases can help prevent unnecessary worry.
| Age | Typical Alignment | What You’ll See |
|---|---|---|
| 0–2 years | Bowlegs (Genu Varum) | Legs curve outward. This is normal. |
| 2–3 years | Neutral to mild valgus | Legs move toward straight, then slight inward knee angle. |
| 3–4 years | Peak knock knees (physiologic valgus) | Knees angle inward (common, usually self‑corrects). |
| 7–8+ years | Adult‑like alignment | Slight inward knee angle (physiologic valgus ~5–7°). Most children “outgrow” knock knees by this age. |
When to See a Doctor (Red Flags)
Consult an Orthopedic Specialist if You Notice:
- Knock knees that persist or worsen after age 7–8 years.
- Asymmetry, where one leg is more affected than the other.
- A significant ankle gap (intermalleolar distance) > 8–10 cm after age 7.
- Associated symptoms like pain, limping, frequent tripping, or difficulty running.
- Short stature, prior trauma/infection near the knee, or sudden onset.
- Family history of bone growth or metabolic disorders.
Symptoms & Common Causes
Symptoms of Knock Knees
- Knees touching or nearly touching with ankles apart.
- Knee pain (often at the front or outer side) or patellofemoral discomfort.
- Frequent tripping or an unusual walking/running pattern (gait).
- Uneven shoe wear.
- Hip, ankle, or foot discomfort due to altered mechanics.
Common Causes
- Physiologic (normal) valgus: most common in early childhood.
- Metabolic bone issues: rickets (vitamin D/calcium deficiency), renal bone disease.
- Post‑traumatic: growth plate disturbance or malunion near the knee.
- Skeletal dysplasias/genetic conditions and ligamentous laxity.
- Obesity can accentuate valgus alignment.
- Less commonly: neuromuscular conditions, prior infection.
Diagnosis Process
- History & physical exam: growth pattern, family history, pain, gait; measure intermalleolar distance and tibiofemoral angle.
- Standing long‑leg X‑ray/EOS: hip‑to‑ankle alignment to locate deformity (femur vs tibia) and quantify mechanical axis deviation.
- Lab tests (if suspected): vitamin D, calcium, phosphate, alkaline phosphatase for rickets/metabolic bone disease.
- Rotational profile or CT only if torsional abnormalities are suspected.
Treatment Options for Children & Adults
Children
- Observation & reassurance: most cases improve naturally.
- Address nutrition: treat vitamin D/calcium deficiency when present.
- Physiotherapy: improves strength and gait mechanics (doesn’t change bone alignment on its own).
- Orthotics/bracing: may improve comfort but rarely correct bony alignment in physiologic valgus.
- Guided growth (hemiepiphysiodesis): minimally invasive plates across one side of the growth plate to gradually correct alignment—best before growth plates close.
- Osteotomy: for severe deformity or skeletally mature teens where guided growth is not possible.
Adults
- Physiotherapy: hip abductors/gluteals and quadriceps strengthening, balance and gait work.
- Activity/weight management and supportive footwear/orthotics for symptom relief.
- Pain relief: NSAIDs as advised; consider targeted injections for associated conditions.
- Realignment osteotomy: distal femoral or proximal tibial osteotomy to shift load and improve mechanics in symptomatic malalignment.
- Knee replacement: considered if advanced arthritis coexists.
Helpful Exercises (guided by a physiotherapist)
- Hip abductor (gluteus medius) strengthening: side‑lying leg raises, banded lateral walks.
- Quadriceps (including VMO) strengthening: mini‑squats, wall sits, step‑ups.
- Hamstring and calf stretches; ankle mobility drills.
- Single‑leg balance and gait retraining.
What to Expect at Your Consultation
- Detailed discussion: symptoms, medical history, growth pattern, and goals.
- Physical examination: leg alignment measurements, gait assessment.
- Imaging review: we’ll explain any X‑rays or scans and what they mean.
- Personalized plan: from observation and physio to guided growth or osteotomy if indicated.
Frequently Asked Questions
Will exercises straighten knock knees?
Exercises improve strength, control, and symptoms but do not change bony alignment. Structural correction in growing children uses guided growth; adults may need osteotomy for realignment when indicated.
Can knock knees cause arthritis?
Significant, persistent valgus can increase stress on the lateral compartment and patellofemoral joint, potentially raising arthritis risk over time. Early assessment helps guide prevention and treatment.
Are braces effective?
Bracing can support comfort and function but rarely corrects bone alignment in physiologic valgus. Corrective options are guided growth (children) or osteotomy (teens/adults) when needed.
When is surgery considered?
When deformity is persistent, progressive, or symptomatic with functional impact, or when imaging shows significant mechanical axis deviation. Choice depends on age, location of deformity, bone quality, and goals.
Need an Expert Opinion?
We use a conservative‑first approach and offer precise alignment planning when surgery is needed. Explore our Orthopedic services or book a consultation.
Further Reading: AAOS OrthoInfo: Knock Knees (Genu Valgum) · NHS: Knock Knees