Prolapsed Intervertebral Disc (PIVD) • Herniated/“Slipped” Disc: Causes, Symptoms, Diagnosis & Treatment
Medically reviewed by Dr. Neelabh, MS (Orthopedics) Educational information only—always consult an Orthopedic specialist for diagnosis and treatment.
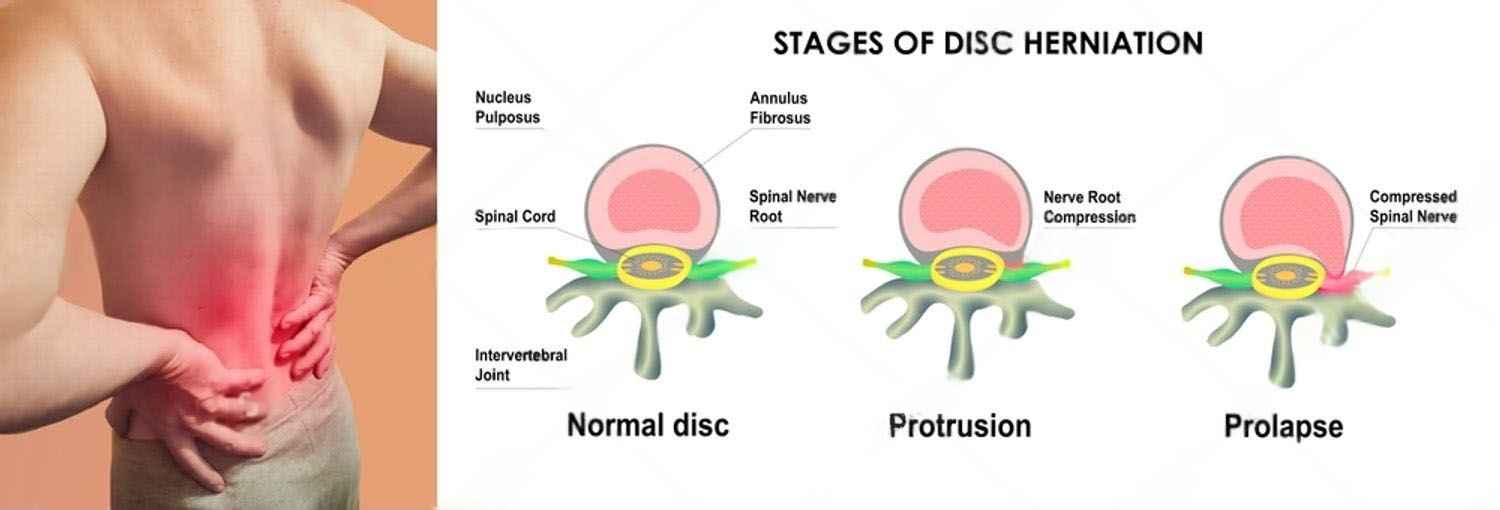
A prolapsed intervertebral disc (PIVD)—also called a herniated disc or “slipped disc”—occurs when part of the disc’s soft center presses through its outer ring and can irritate nearby nerves. This may cause back or neck pain and radiating pain into an arm or leg.
On this page
Disc Anatomy (Simple)
- Nucleus Pulposus: The soft, gel-like center that absorbs shock and load.
- Annulus Fibrosus: The tough outer ring made of strong collagen layers.
- Cartilaginous Endplates: Thin layers that attach the disc to the vertebral bodies above and below.
Most of the disc is avascular (lacks a direct blood supply), and only the outer annulus is innervated, which is why tears can be painful.
Common Causes & Risk Factors
- Age-Related Degeneration: The most common cause; discs naturally lose water content and flexibility over time.
- Loading/Strain: Improper heavy lifting, sudden awkward twisting, or prolonged vibration (e.g., long-distance driving).
- Genetic Predisposition & Smoking: Both are linked with accelerated disc degeneration.
- Injury/Trauma: A fall or direct blow to the spine can precipitate herniation.
Symptoms of a Herniated Disc
Symptoms vary based on the location of the herniation:
- Lumbar (Low Back) Herniation: Low back pain, sciatica (buttock/leg pain radiating below the knee), numbness/tingling, or weakness in the leg/foot. Often worse with coughing, sneezing, or prolonged sitting.
- Cervical (Neck) Herniation: Neck pain with arm pain/numbness in a dermatomal pattern (brachialgia), possible hand weakness or grip changes.
Red Flags—Seek Urgent Care
Seek immediate medical attention if you experience:
- New bowel or bladder dysfunction, urinary retention, or numbness in the “saddle” area (possible Cauda Equina Syndrome).
- Rapidly progressive weakness (e.g., new foot drop in the leg or hand weakness in the arm).
- Severe, unremitting pain with fever, unexplained weight loss, history of cancer, significant trauma, or IV drug use.
Diagnosis—What to Expect
- History & Physical Exam: Dermatomal sensory testing, muscle strength, and reflexes; Straight Leg Raise (lumbar) or Spurling’s (cervical) may reproduce symptoms.
- Imaging (MRI): The gold standard when symptoms are severe, atypical, persist beyond ~4–6 weeks despite care, or if red flags are present. Routine early MRI is often unnecessary for simple back pain.
- Other tests: X‑rays assess alignment but don’t show discs; CT/myelogram if MRI is contraindicated.
Treatment Pathway: From Conservative to Surgical
Most herniated discs improve with conservative care within 6–12 weeks.
Step 1: Conservative (First-Line) Care
- Activity Modification: Stay gently active; avoid strict bed rest. Limit positions/loads that aggravate symptoms.
- Medications: NSAIDs/acetaminophen; short courses of neuropathic agents (e.g., gabapentin) for radicular pain; brief oral steroids in selected cases (doctor-guided).
- Physical Therapy: McKenzie‑based extension (lumbar), posture and scapular work (cervical), core/hip strengthening, nerve glides, and graded return to activity.
Step 2: Interventional Pain Management
- Epidural Steroid Injections: Interlaminar or transforaminal injections can reduce inflammation around the irritated nerve and provide a window of relief to progress rehab.
Step 3: Surgical Consultation
Surgery is considered in select cases when non-operative care fails or for urgent conditions.
- Indications: Cauda Equina Syndrome, progressive motor deficit, or intractable radicular pain significantly impacting life after 6–12 weeks of appropriate conservative care.
- Common Procedures: Lumbar microdiscectomy or endoscopic discectomy; cervical ACDF (fusion), posterior foraminotomy (selected cases), or disc arthroplasty in suitable patients.
- Outcomes: Surgery primarily relieves leg/arm pain faster; axial back/neck ache may recover more gradually with rehab.
Recovery & Prevention
- Rehab plan: Progress from pain control to flexibility, core/hip strength, nerve glides, then endurance and return-to-activity.
- Ergonomics: Neutral spine sitting/standing, frequent micro‑breaks, proper lifting mechanics.
- Stay active: Walking, cycling, or swimming 3–5×/week; avoid prolonged bed rest.
- Risk reduction: Stop smoking, maintain a healthy weight, build baseline strength and flexibility.
- Pain control: NSAIDs/acetaminophen as advised; opioids are generally not first‑line for disc pain.
A Surgeon’s Perspective by Dr. Neelabh
“My first goal is always to help patients recover without surgery. For most herniated discs, a combination of targeted physical therapy, medication, and time is highly effective. Surgery has a clear role, but it’s reserved for those with severe nerve compression or pain that doesn’t improve. We make that decision together, based on your symptoms, MRI findings, and lifestyle goals.”
What to Expect at Your Consultation
- Detailed Discussion: Your symptoms, medical history, and goals.
- Physical Examination: Spine, nerve function, and movement assessment.
- Imaging Review: We explain MRI or other scan findings in simple terms.
- Personalized Plan: Clear diagnosis and a tailored plan—from observation and physio to injections or surgery, if indicated.
Frequently Asked Questions
How long does a herniated disc take to heal?
Many patients feel significantly better within 6–12 weeks with conservative care. Nerve pain often improves before numbness fully resolves.
Do I need an MRI right away for my back pain?
Not usually. An MRI is appropriate if there are red flags, or if significant symptoms persist beyond several weeks despite proper care.
Will exercises push the disc back in?
Exercises don’t physically “push” the disc back, but they can reduce pain, centralize symptoms, improve function, and support natural healing by optimizing mechanics.
When is surgery the best option?
For progressive weakness, cauda equina, or refractory nerve pain affecting daily life despite good conservative care. Your surgeon will review the risks/benefits for your case.
Need a Spine Opinion?
We follow a conservative-first approach and personalize your plan to get you back to your life. Explore our Orthopedic services or book a consultation.
Further Reading: AAOS: Herniated Disk · NHS: Slipped Disc
it was because of image file name, please write the whole content to paste it in divi text module?