Hip Arthritis: Symptoms, Causes, Diagnosis & Treatment Options
Medically reviewed by Dr. Neelabh, MS (Orthopedics) Educational information only—always consult a qualified Orthopedic specialist for diagnosis and treatment.
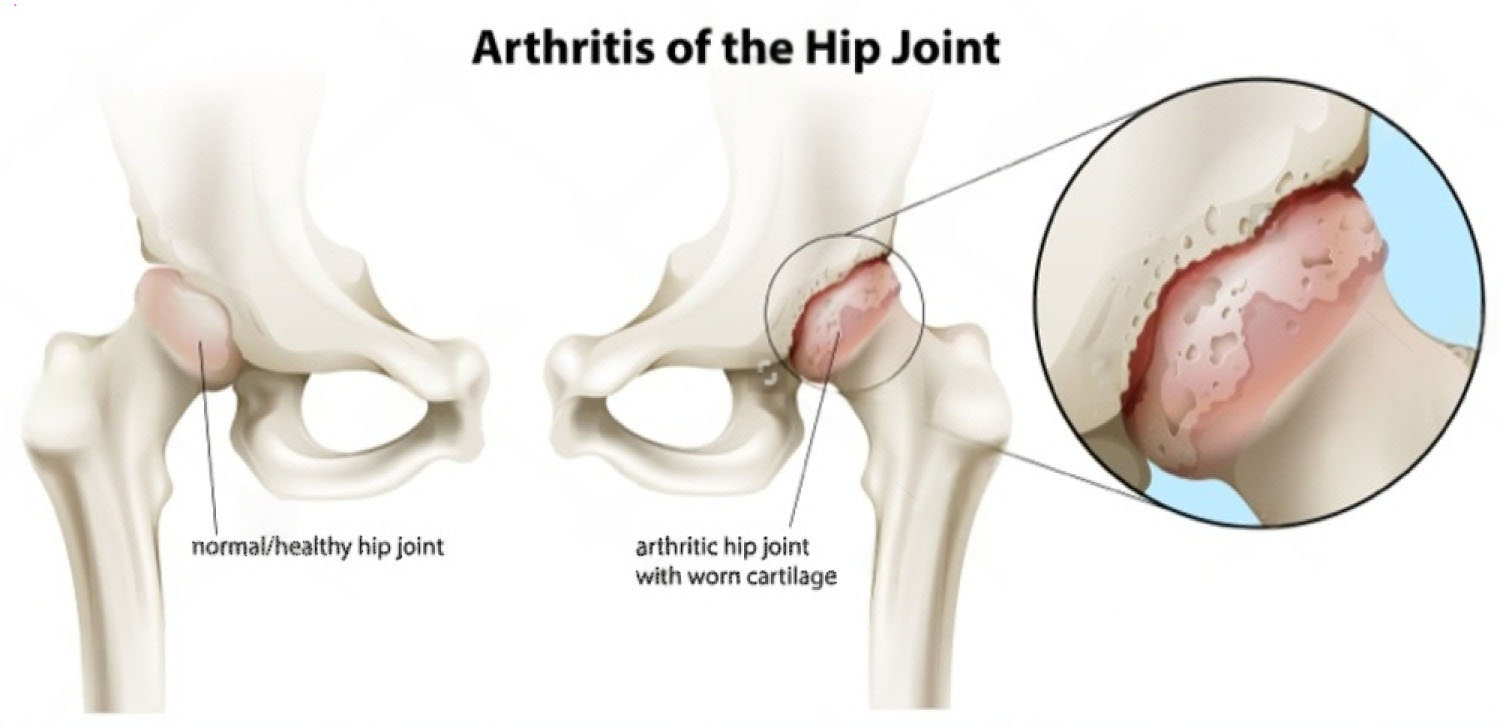
Hip arthritis (most commonly osteoarthritis) occurs when the smooth cartilage that cushions the hip joint wears down, leading to pain, stiffness, and reduced mobility. With the right plan—from conservative care to surgery—most patients can return to an active, independent life.
On this page
Hip Arthritis Symptoms
- Groin pain (most common), sometimes buttock or outer thigh pain.
- Morning stiffness or “start‑up” pain after periods of rest.
- Pain with activity: walking, stairs, getting in/out of a car; often a limp.
- Reduced range of motion: difficulty putting on socks/shoes.
- Activity‑related swelling or tenderness around the hip.
When to See a Doctor (Urgent and Prompt Care)
- After a fall/injury: inability to bear weight, visible deformity, or leg shortening (possible fracture).
- Fever, redness, warmth over the hip with severe pain (possible joint infection).
- Sudden severe groin pain with inability to move the hip.
- Rapidly worsening night/rest pain or unintentional weight loss.
Common Causes and Risk Factors
- Primary (age‑related) osteoarthritis.
- Inflammatory arthritis: rheumatoid arthritis, ankylosing spondylitis.
- Secondary causes: Avascular necrosis (AVN), post‑traumatic arthritis, post‑infection.
- Structural issues: femoroacetabular impingement (FAI), developmental dysplasia.
- Genetics, obesity, high joint loads, certain occupations/sports.
How Hip Arthritis is Diagnosed
- History & physical exam: pain location, gait, range of motion, impingement tests.
- X‑rays (first‑line): AP pelvis and lateral hip to assess joint space, osteophytes, cysts.
- MRI (selective): suspected AVN; early disease not seen on X‑ray; labral/FAI evaluation.
- Rule‑outs: lumbar spine referral, greater trochanteric pain syndrome, hernia.
Hip Arthritis Treatment Pathway (Step-by-Step)
1) Conservative Management
- Education & activity modification: joint‑friendly activities (walking, cycling, swimming); avoid prolonged sitting and deep flexion if painful.
- Physiotherapy: hip abductors/gluteals and core strengthening, gait/balance, flexibility.
- Weight management and cane use (in the opposite hand) to reduce joint load.
- Medications: NSAIDs/acetaminophen as advised; topical NSAIDs may help peri‑trochanteric pain.
2) Image‑Guided Injections (Selected Cases)
- Corticosteroid injection: can reduce pain short‑term (weeks to months) to help progress rehab.
- Viscosupplementation (hyaluronic acid): mixed evidence in the hip; consider after shared discussion.
3) Arthroscopy (Limited Role)
Hip arthroscopy can treat FAI/labral tears in patients without established arthritis. It is not generally beneficial once moderate–severe osteoarthritis is present.
4) Surgical Replacement
- Total Hip Replacement (THR): the gold standard when pain and functional limits persist despite optimized conservative care, or when X‑rays show advanced arthritis. THR replaces the damaged ball and socket with durable components and reliably relieves pain. Learn more about Total Hip Replacement.
A Surgeon’s Perspective by Dr. Neelabh
“We always begin with a comprehensive conservative plan—physiotherapy, load management, and medication. When pain continues to limit your life and X‑rays confirm advanced arthritis, a Total Hip Replacement offers the most predictable, long‑term relief. This is a shared decision, always tailored to your personal goals.”
What to Expect at Your Consultation
- Detailed discussion: symptoms, medical history, functional goals.
- Physical examination: gait, range of motion, impingement tests.
- Imaging review: we’ll explain your X‑rays/MRI and what they mean.
- Personalized plan: from physiotherapy and injections to THR if indicated.
Recovery, Activity & Prevention
- After THR: walking often same/next day; driving 2–6 weeks (side/vehicle dependent); desk work ~2–4 weeks; heavy work longer.
- Physio‑led rehab: gait training, strength, and balance reduce limp and improve outcomes.
- Joint care: maintain healthy weight, keep hips strong/flexible, and choose joint‑friendly activities.
Frequently Asked Questions
What are the alternatives to hip replacement?
For early to moderate hip arthritis, a structured program of physiotherapy, weight management, activity modification, and NSAIDs can be very effective. Injections can also provide temporary relief. Hip replacement is reserved for advanced cases where these measures no longer control pain and functional decline.
What is the best exercise for hip arthritis?
Low‑impact aerobic exercises (walking, cycling, swimming) combined with targeted strengthening for the hip abductors and core. A physiotherapist can create a personalized and safe plan for you.
How long does a hip replacement last?
With modern implants and proper surgical technique, many total hip replacements function well beyond 15–20 years.
Need an Expert Opinion?
We use a conservative‑first approach and offer personalized surgical options when needed. Explore our Orthopedic services or book a consultation.
Further Reading: AAOS: Hip Osteoarthritis · NICE OA Guideline (NG226)