Partial Hip Replacement in Delhi (Bipolar Hemiarthroplasty)
Partial Hip Replacement in Delhi with Dr. Neelabh focuses on timely surgery, modern implants (bipolar/unipolar), and a clear early‑mobilisation plan coordinated with your physiotherapist—so you can get back on your feet safely.
Fracture‑focused care • Cemented/uncemented stems • We do not provide in‑house physiotherapy—protocols shared with your physio. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)

Fracture expertise
Focused care for femoral neck fractures in older adults and select AVN/pathologic cases.
Bipolar options
Bipolar heads reduce acetabular friction; choice tailored to bone and activity.
Early mobilisation
Weight‑bearing as tolerated in many cases—under a written protocol your physio follows.
Clear guidance
From admission to discharge and follow‑up—know what to expect at each step.
What is Partial Hip Replacement in Delhi?
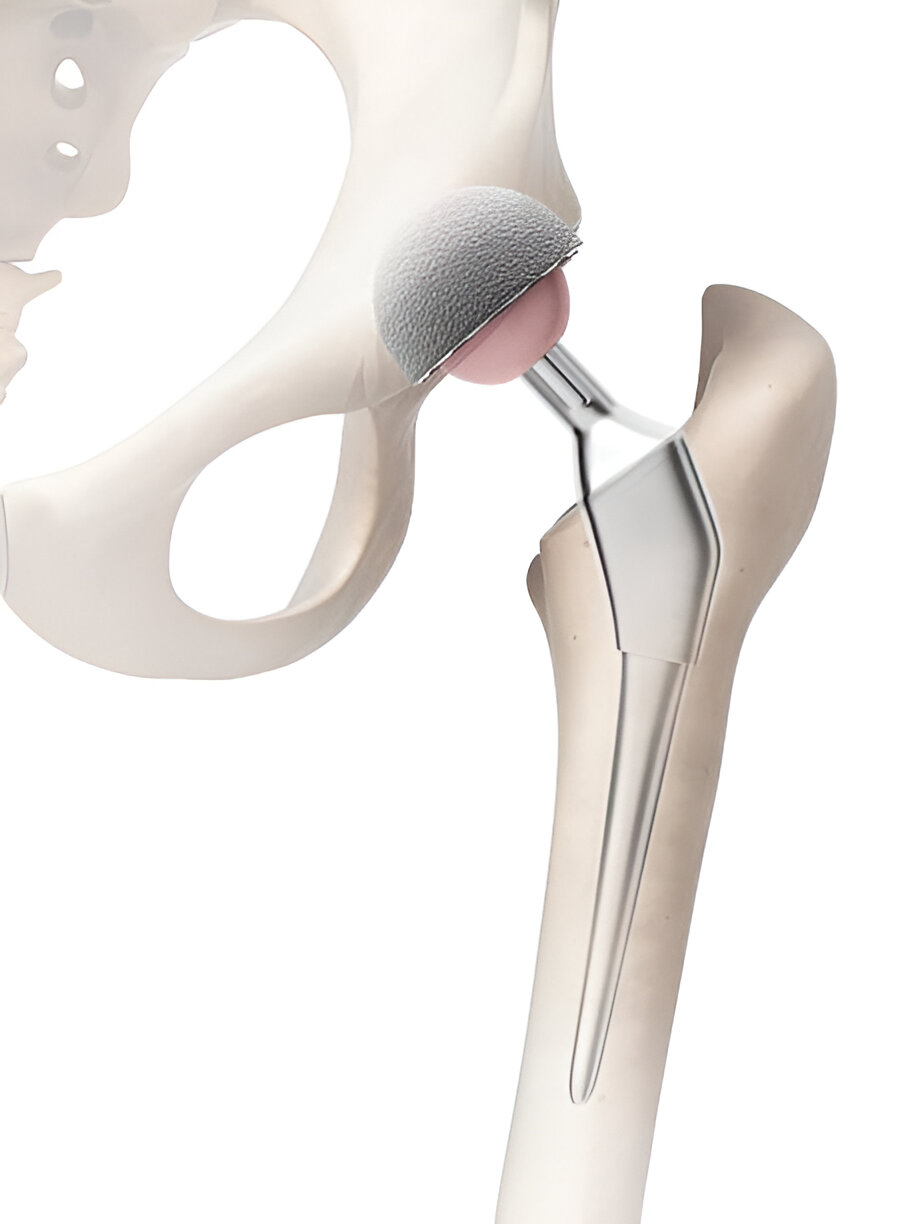
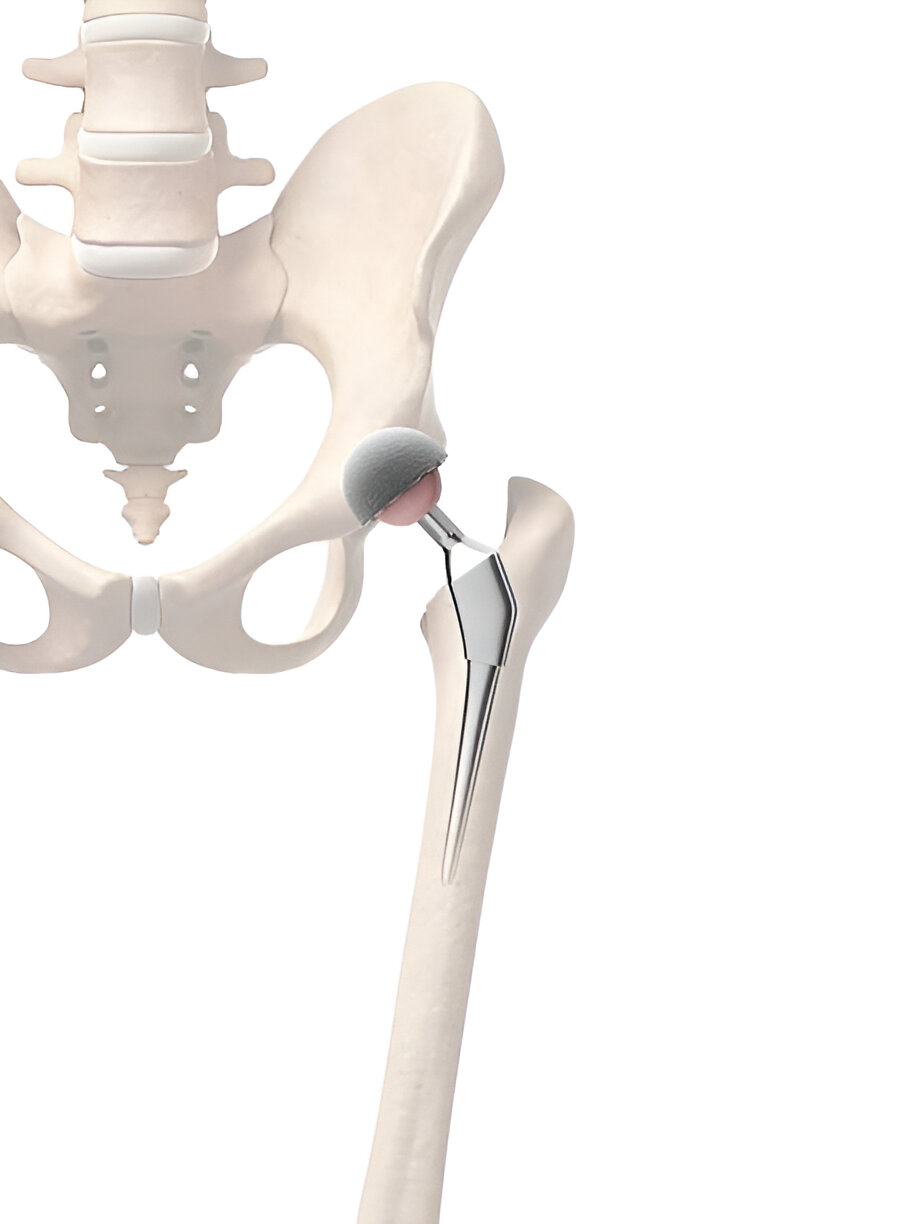
Partial Hip Replacement—also called hip hemiarthroplasty—replaces the damaged femoral head while keeping the natural socket (acetabulum). In a bipolar hip replacement, the prosthetic head has an inner and outer bearing to allow motion between the head and the shell, potentially reducing acetabular wear compared with a unipolar design.
Compared with total hip replacement (THR), partial replacement is often chosen for displaced femoral neck fractures in older adults, where a quicker operation and early walking are priorities and the socket cartilage is acceptable.
Who is a Good Candidate?
Displaced femoral neck fracture
Common in older adults following a fall.
Limited socket damage
Acetabular cartilage is acceptable at surgery.
Medical considerations
When a shorter operation is safer due to comorbidities.
Functional goals
Early standing/walking with assistive devices as needed.
If imaging shows significant socket arthritis or high activity goals, total hip replacement may be advised instead.
Benefits
- Timely surgery designed for early, safe mobilisation
- Often shorter operative time vs THR in fracture settings
- Bipolar head may reduce acetabular wear vs unipolar
- Clear post‑op pathway coordinated with your physiotherapist
Risks & How We Reduce Them
- Infection, blood clots, dislocation, leg length difference
- Acetabular cartilage wear over time (may require conversion to THR)
- Medical risks related to age/comorbidities
We reduce risk with peri‑operative antibiotics, DVT prevention, meticulous technique, and early but protected mobilisation.
Implants & Options
- Cemented vs uncemented stems: Choice depends on bone quality, fracture pattern, and medical status.
- Bipolar vs unipolar heads: Bipolar provides an additional inner bearing; your case guides selection.
- Approach: Posterolateral or anterolateral—selected for stability and tissue preservation.
All options are discussed transparently so you can make an informed decision.
How Partial/Bipolar Hip Replacement is Performed
- Anaesthesia & approach: Spinal/epidural or general anaesthesia; posterolateral or anterolateral approach.
- Femoral head removal: The fractured head is removed; the canal is prepared.
- Stem & head placement: Cemented or uncemented stem with bipolar/unipolar head sized for stability.
- Stability check: Leg length, offset, and range of motion tested to minimise dislocation risk.
- Closure & pathway: Wound closed; mobilisation and hip precautions reviewed.
Recovery Timeline
- Day 0–1: Sit/stand with assistance; step‑to walking as safe.
- Week 1–2: Progress walking aids; swelling and wound care.
- Week 3–6: Improve strength and balance; many return to light activities.
- Month 3–6: Advance to community walking and low‑impact routines.
We do not provide in‑house physiotherapy. You’ll receive a written rehab protocol and we’ll coordinate with your chosen physiotherapist (external referrals available).

Where to Consult Dr. Neelabh
Jeewan Hospital
Jeewan Hospital, Metro Station, 2-B, Pusa Rd, opp. Pillar No.-107, 108, Block B, Karol Bagh, New Delhi, Delhi, 110005
🕓 3:00 PM – 4:00 PM
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Clinic Intermed
Clinic Intermed, 38/16, Block 38, East Patel Nagar, Patel Nagar, New Delhi, Delhi, 110008
🕓 6:00 PM – 8:00 PM
Timings may vary—please call +91-9810117204 to confirm.
Cost & Insurance
Costs depend on implant choice (cemented/uncemented, bipolar/unipolar), facility and anaesthesia fees, and insurance coverage. We verify benefits and provide a transparent estimate before scheduling your Partial Hip Replacement in Delhi.
- Insurance pre‑authorisation & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

How to Prepare
Medical clearance
Pre‑op evaluation, labs, ECG, and imaging (X‑ray ± CT) as needed.
Medication review
Guidance on blood thinners, diabetes medicines, and supplements.
Prehab (external)
We recommend prehab with your physiotherapist for transfer training and safe gait.
Home setup
Non‑slip footwear, remove tripping hazards, arrange support for daily tasks.
Healthy habits
Stop smoking, optimise blood sugar/nutrition, maintain skin health.
Frequently Asked Questions
Partial vs Total Hip Replacement—how do you decide?
When will I start walking?
Cemented or uncemented—what’s better?
Could I need a future THR?
Do you provide physiotherapy?
When can I drive or return to work?
Need timely fracture care?
Let’s design a safe surgical and recovery plan tailored to you.
