Revision Joint Replacement in Delhi (Knee & Hip)
Revision Joint Replacement in Delhi addresses failed or painful knee/hip replacements due to loosening, wear, infection, instability, or fracture. We plan each case meticulously and share a clear recovery protocol with your physiotherapist. We do not provide in‑house physiotherapy.
Complex revision expertise • Advanced implants (stems, cones, augments) • Infection & instability solutions. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)

Complex revision focus
Loosening, wear/osteolysis, instability, infection (PJI), periprosthetic fracture.
Advanced reconstruction
Long stems, cones/sleeves, augments, constrained liners, modular options.
Infection strategies
DAIR, one‑stage, or two‑stage revision as indicated—culture‑guided antibiotics.
Clear rehab protocol
We coordinate with your physiotherapist; written milestones provided.
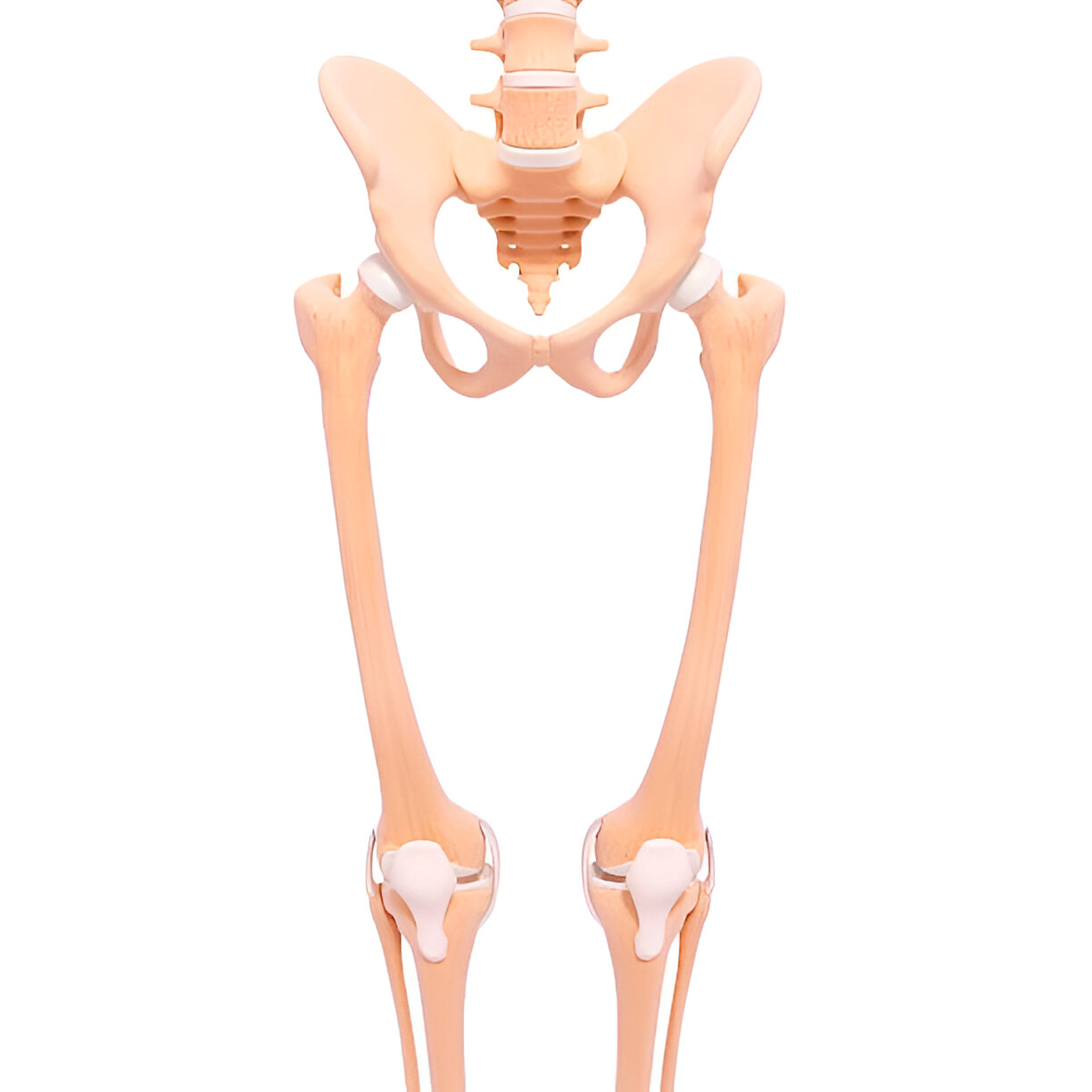
What is Revision Joint Replacement in Delhi?
Revision joint replacement is surgery to correct problems after a previous knee or hip replacement. It may involve exchanging the liner, replacing one component, or performing a full revision with specialised implants to restore stability and function.
Revisions are more complex than primary surgery and require careful diagnosis, planning, and reconstruction techniques to address bone loss and soft‑tissue balance.

When Is Revision Needed?
Aseptic loosening
Component loosening and osteolysis/wear over time.
Instability/stiffness
Recurrent giving‑way, malalignment, or limited motion.
Infection (PJI)
Pain, swelling, sinus, or raised markers; requires targeted strategy.
Periprosthetic fracture
Fracture around the implant needing fixation and/or revision.
Component issues
Malposition, wear, patellofemoral or extensor mechanism problems.
Failed previous revision
Persistent pain or dysfunction after earlier surgery.
Evaluation & Planning
- Imaging: X‑rays (standing/alignment); CT for bone loss/rotation; long‑leg views for knee; specialised views for hip.
- Infection screen: ESR/CRP, joint aspiration, cell count, cultures; MSIS criteria when needed.
- Bone loss mapping: AORI (knee) / Paprosky (hip) to plan stems, cones, sleeves, and augments.
- Risk optimisation: Anaemia, diabetes, nutrition, skin, and smoking cessation.
A precise diagnosis guides whether limited exchange or full revision is safest.
Treatment Options
Liner/isolated exchange
If components are well fixed and aligned; addresses wear/instability in select cases.
Component revision
Replace loose or malpositioned parts; restore alignment and balance.
Full revision
Stems, augments, cones/sleeves to manage bone loss; constrained liners if needed.
Fracture + revision
Periprosthetic fracture fixation combined with revision for stability.
Salvage options
In rare complex failures, staged or alternative procedures may be required.
Infection Management (PJI)
- DAIR: Debridement, Antibiotics, and Implant Retention for early, well‑selected cases.
- One‑stage revision: Exchange components in one surgery for defined organisms/patients.
- Two‑stage revision: Remove implants, place spacer, targeted antibiotics, later reimplantation.
Approach depends on organism, chronicity, fixation, soft tissues, and patient factors—planned with microbiology input.

How Revision Surgery is Performed
- Anaesthesia & approach: Spinal/epidural or general; prior scars considered for safe access.
- Component removal & debridement: Extract loose parts, remove cement, manage osteolysis.
- Reconstruction: Stems, augments, cones/sleeves to address bone loss; restore alignment and joint line.
- Stability & tracking: Ligament balance for knees; offset/leg length and stability for hips.
- Closure & pathway: Wound closed; DVT prevention, antibiotics as indicated; written rehab protocol.
Recovery Timeline
- Day 0–2: Stand/walk with assistance; start gentle, safe range‑of‑motion.
- Week 1–3: Swelling control; progress walking aids; wound checks.
- Week 4–8: Strength and motion improve; many resume light activities.
- Month 3–6: Low‑impact routines; gradual return to community function.
Revision recovery varies by complexity and bone quality. We do not provide in‑house physiotherapy. You’ll receive a written rehab protocol and we coordinate with your chosen physiotherapist.

Cost & Insurance
Costs depend on diagnosis (loosening, infection, fracture), implant selection (stems, cones, augments), need for staged procedures, facility and anaesthesia fees, and coverage. We verify benefits and provide a transparent estimate before scheduling your Revision Joint Replacement in Delhi.
- Insurance pre‑authorisation & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

How to Prepare
Medical clearance
Pre‑op evaluation, labs, ECG; infection screen when indicated.
Medication review
Guidance on blood thinners, diabetes medicines, and supplements.
Optimise health
Treat anaemia, control sugars, stop smoking, maintain skin integrity.
Prehab (external)
We recommend prehab with your physiotherapist: safe transfers and gait.
Home setup
Remove tripping hazards; arrange support; prepare a recovery space.
Where to Consult Dr. Neelabh
Jeewan Hospital
Jeewan Hospital, Metro Station, 2-B, Pusa Rd, opp. Pillar No.-107, 108, Block B, Karol Bagh, New Delhi, Delhi, 110005
🕓 3:00 PM – 4:00 PM
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Clinic Intermed
Clinic Intermed, 38/16, Block 38, East Patel Nagar, Patel Nagar, New Delhi, Delhi, 110008
🕓 6:00 PM – 8:00 PM
Timings may vary—please call +91-9810117204 to confirm.
Frequently Asked Questions
How is revision different from primary replacement?
Will a revision last as long as a primary?
Is revision always possible?
Do you provide physiotherapy?
How do you detect infection?
When can I get back to daily activities?
Need an expert opinion on a painful joint replacement?
Let’s design a safe, personalised revision plan.
