Osteoporosis and Metabolic Bone Disease in Delhi
Osteoporosis and Metabolic Bone Disease in Delhi with Dr. Neelabh focuses on accurate diagnosis, fracture‑risk assessment, medication plans tailored to your profile, and practical prevention strategies—backed by a clear home‑exercise and safety protocol coordinated with your chosen physiotherapist. We do not provide in‑house physiotherapy.
Precise DXA‑based diagnosis • FRAX fracture‑risk profiling • Medication + lifestyle plan • Fall‑prevention & home safety. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)
Accurate diagnosis
DXA scanning, vertebral fracture assessment, and targeted labs to uncover causes.
Tailored therapy
Bisphosphonates, denosumab, or anabolic agents when indicated—plus nutrition & safety.
Fragility fracture care
Rapid surgical triage when needed and a secondary‑prevention plan to stop the next fracture.
External physio coordination
We share written exercise protocols; we do not provide in‑house physiotherapy.
About Osteoporosis & Bone Health
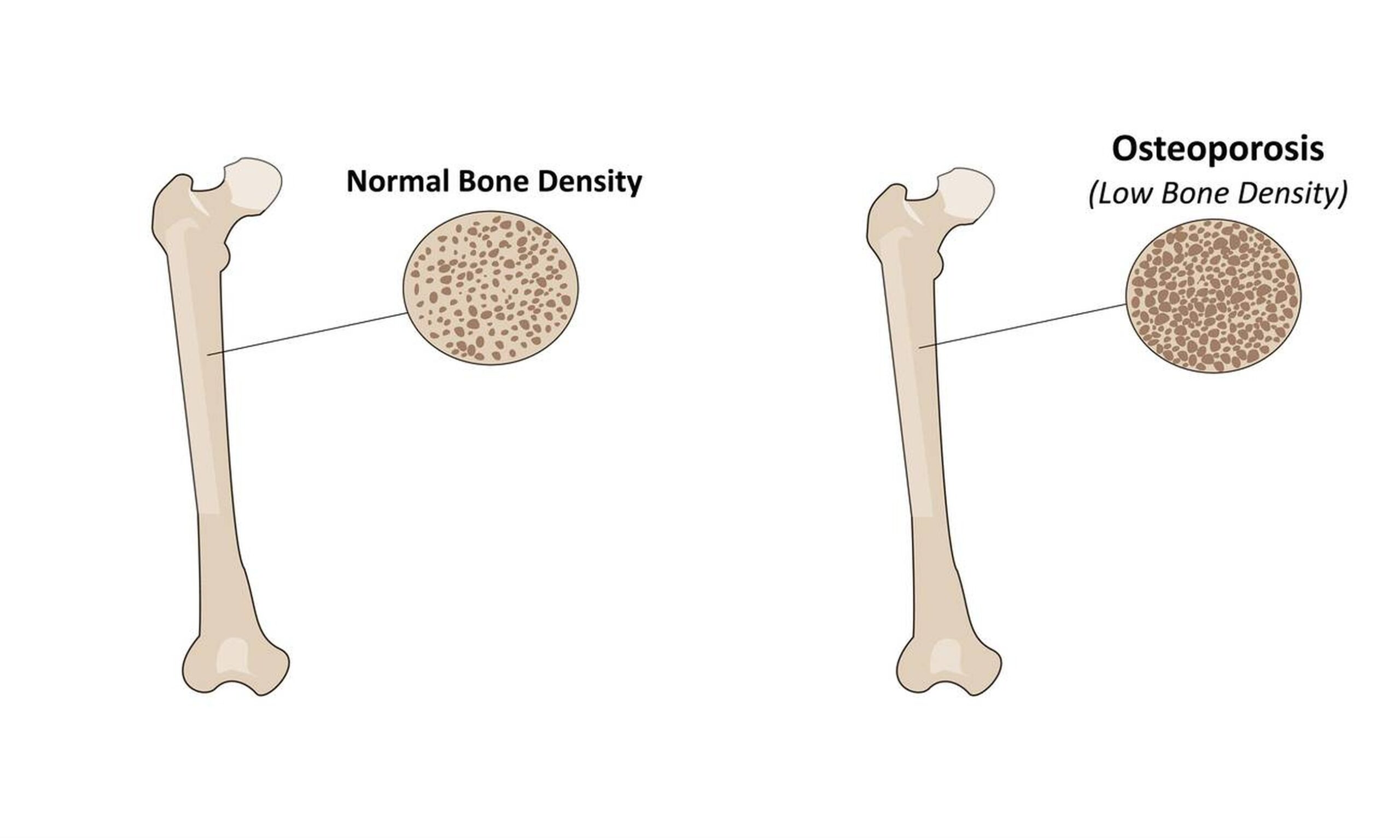
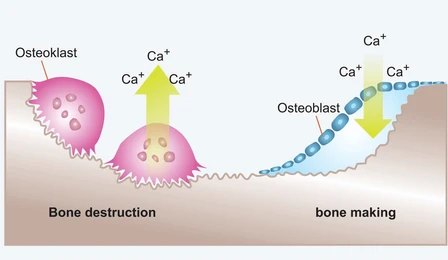
Osteoporosis is a condition of low bone mass and structural deterioration that increases fracture risk. Bone is a living tissue—constantly remodelled by cells that remove old bone and create new bone. Ageing, hormonal changes (especially post‑menopause), inactivity, nutrient deficiencies, and medical conditions can shift this balance, making bones fragile.
Metabolic bone disease is a broader term covering conditions that disrupt bone turnover or mineralisation, such as osteomalacia (vitamin D deficiency), hyperparathyroidism, Paget’s disease, and steroid‑induced bone loss. These disorders can cause pain, deformity, or fractures—and require targeted evaluation and therapy.
Our goal is simple: reduce your fracture risk and keep you moving. That means a precise diagnosis, an effective treatment plan, and practical steps you can implement at home.
Who Is at Risk
Age & sex
Women after menopause; men over 70. Earlier risk with family history.
Low BMI & inactivity
Sedentary lifestyle, prolonged bed rest, or low body weight.
Nutrition
Low calcium/protein intake; vitamin D deficiency; excessive alcohol.
Medications
Long‑term steroids, some anti‑seizure meds, aromatase inhibitors, PPIs.
Medical conditions
Thyroid/parathyroid disease, CKD, RA, malabsorption, hypogonadism.
Fracture history
Any low‑trauma (fragility) fracture after age 50 signals higher risk.
Red flags: sudden back pain with height loss, multiple low‑trauma fractures, or prolonged steroid use—seek evaluation.
Evaluation & Diagnosis
- DXA scan: Measures bone mineral density (BMD) at hip/spine. T‑score ≤ −2.5 indicates osteoporosis; −1.0 to −2.5 is osteopenia.
- Vertebral Fracture Assessment (VFA): Lateral spine imaging (via DXA) to detect silent compression fractures.
- FRAX risk profiling: 10‑year major osteoporotic and hip fracture risk—guides treatment decisions in osteopenia.
- Laboratory tests: Calcium, phosphate, 25‑OH vitamin D, PTH, thyroid, renal/liver profile; coeliac screen in select cases; bone turnover markers for certain scenarios.
- Secondary causes: Review medications and conditions (endocrine, rheumatologic, renal, GI) that accelerate bone loss.
Diagnosis is not only about a T‑score—it’s about your fracture risk today and in the next 10 years. We combine imaging, labs, and clinical factors to create a plan that meets your goals.

Metabolic Bone Diseases We Manage
Osteomalacia (Vit D deficiency)
Soft bones from impaired mineralisation—bone pain, muscle weakness; corrected with vitamin D/calcium and cause‑specific care.
Hyperparathyroidism
Excess PTH draws calcium from bone; may need endocrine/surgical management plus bone‑protective therapy.
Paget’s disease
Focal high‑turnover bone—pain, deformity, elevated ALP; responds to specific bisphosphonates in symptomatic cases.
Glucocorticoid‑induced bone loss
Steroids accelerate resorption—early treatment and prevention are key.
CKD‑related bone disease
Mineral metabolism disorders with fracture risk—co‑managed with nephrology.
Men’s bone health
Hypogonadism, alcohol, smoking, and steroids—often under‑recognised but treatable.
We coordinate with endocrinology/nephrology where appropriate for comprehensive care.
Treatment Plan
Nutrition & supplements
Aim for total calcium intake ~1,000–1,200 mg/day (diet + supplement as needed) and vitamin D to maintain 25‑OH vitamin D typically >30 ng/mL. Adequate protein (≈1.0–1.2 g/kg) supports muscle and bone.
Exercise (external physio)
We provide a written home program prioritising posture, balance, and safe strength work. We do not provide in‑house physiotherapy; we coordinate with your chosen physiotherapist and can recommend external partners.
Medications
Bisphosphonates (alendronate, risedronate, zoledronic acid) reduce fracture risk; consider drug holidays in low‑risk stable patients after a defined period. Denosumab is effective; avoid stopping abruptly without a transition plan. Anabolic agents (teriparatide, abaloparatide, romosozumab—where available) are considered for very high risk or multiple fractures, typically followed by antiresorptive therapy.
Dental & safety
Complete dental checks before IV bisphosphonates or denosumab when possible; maintain oral hygiene. We discuss rare risks (ONJ, atypical femoral fractures) and monitor appropriately.
Sequential therapy
In very high‑risk patients, start with an anabolic agent then consolidate with an antiresorptive for durable gains. We individualise duration and sequencing.
Your plan is personalised—based on BMD, fracture history, FRAX, age, kidney function, and preferences.
Fragility Fractures: Repair & Prevention
Hip, spine, wrist, or shoulder fractures after a minor fall are common consequences of osteoporosis. We prioritise timely fracture management—surgical where indicated—and immediate secondary prevention so the first fracture is the last.
- Surgical triage: Early fixation or hip replacement (partial/total) when appropriate to enable safe mobilisation.
- Pain & function: Medication review, braces when helpful, and a protected mobilisation plan.
- Secondary prevention: Initiation of bone medication, vitamin D/calcium, home‑safety measures, and written exercise program coordinated with your physiotherapist.
We do not provide in‑house physiotherapy; we coordinate with your therapist for safe, progressive recovery.

Falls & Home Safety
Home setup
Remove loose rugs, improve lighting (especially corridors/bathrooms), add grab bars and non‑slip mats, keep essentials at waist height.
Vision & footwear
Regular eye checks; supportive, non‑slip shoes; avoid walking in socks on smooth floors.
Medications
Review sedatives and blood pressure meds that increase falls; avoid excessive alcohol.
Balance training
Written balance drills and posture cues; progress under the guidance of your physiotherapist.
Monitoring & Follow‑Up
- DXA schedule: Typically every 1–2 years (earlier if clinical changes or high‑risk transitions).
- Lab checks: Vitamin D, calcium, renal profile; additional labs if therapy changes.
- Adherence & tolerance: Confirm medication technique (e.g., oral bisphosphonates) and address side effects.
- Re‑risking: Update FRAX and clinical factors; adjust therapy or consider sequential strategies.
If stopping denosumab, plan a follow‑on antiresorptive to avoid rebound bone loss and fractures.

Cost & Insurance
Costs depend on evaluation (DXA, labs), diagnosis, and treatment plan (medications or surgical care if a fracture is present), plus facility and pharmacy fees. We verify benefits and provide a transparent estimate before scheduling your Osteoporosis and Metabolic Bone Disease in Delhi visit.
- Insurance pre‑authorisation & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

How to Prepare
Bring prior records
DXA reports, spine/hip X‑rays, lab tests, and a list of medicines/supplements.
Meal/fasting notes
Some labs may need fasting; we’ll advise when scheduling.
Dental check
If IV therapy is planned, complete dental evaluation when possible.
Exercise partner
Identify a physiotherapist/gym coach who can help you follow the written program.
Questions & goals
Note your priorities (e.g., reduce falls, avoid surgery, return to walking distance).
Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91-9810117204 to confirm.
Frequently Asked Questions
Do I need treatment if I have osteopenia, not osteoporosis?
How long will I need bone medication?
Can exercise rebuild my bones?
Do you provide physiotherapy?
When should I repeat my DXA?
Are there side effects to bone medications?
Ready to strengthen your bones and reduce fracture risk?
Let’s design a plan tailored to your diagnosis, lifestyle, and goals.
