Paediatric Orthopedics in Delhi (Children’s Bone & Joint Care)
Paediatric Orthopedics in Delhi with Dr. Neelabh focuses on accurate diagnosis, child‑friendly care, and practical treatment plans for newborns to adolescents—covering hip, foot, limb, spine, and sports injuries. We share written home‑exercise and recovery protocols with your chosen physiotherapist. We do not provide in‑house physiotherapy.
Child‑centred clinics • Growth‑aware decisions • Evidence‑based care • Family education. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)

Child‑friendly approach
Gentle handling, clear explanations, and age‑appropriate strategies for children and teens.
Growth‑plate focus
Plans that respect growth and future alignment—avoiding overtreatment.
Least invasive first
Casting/bracing and guided‑growth where possible; surgery when necessary.
External physio coordination
We share written rehab protocols with your physiotherapist; no in‑house physio.
About Paediatric Orthopaedics
Children are not just “small adults.” Their bones grow, their ligaments are more elastic, and their joints remodel over time. Paediatric orthopaedics specialises in conditions that affect growth, development, and movement—from newborn hip screening to adolescent sports injuries. The aim is to restore comfortable, confident movement while protecting growth plates and future alignment.
We favour least‑invasive options first: observation, activity guidance, casting/bracing, and targeted injections in select cases. When surgery is needed, we use techniques suited to growing bones—guided growth, percutaneous fixation, and child‑appropriate implants—so kids can get back to play and learning as safely and quickly as possible.

Conditions We Treat
Newborn & infant hip
Developmental Dysplasia of the Hip (DDH)—screening, ultrasound, Pavlik harness, closed/open reduction as needed.
Foot & ankle
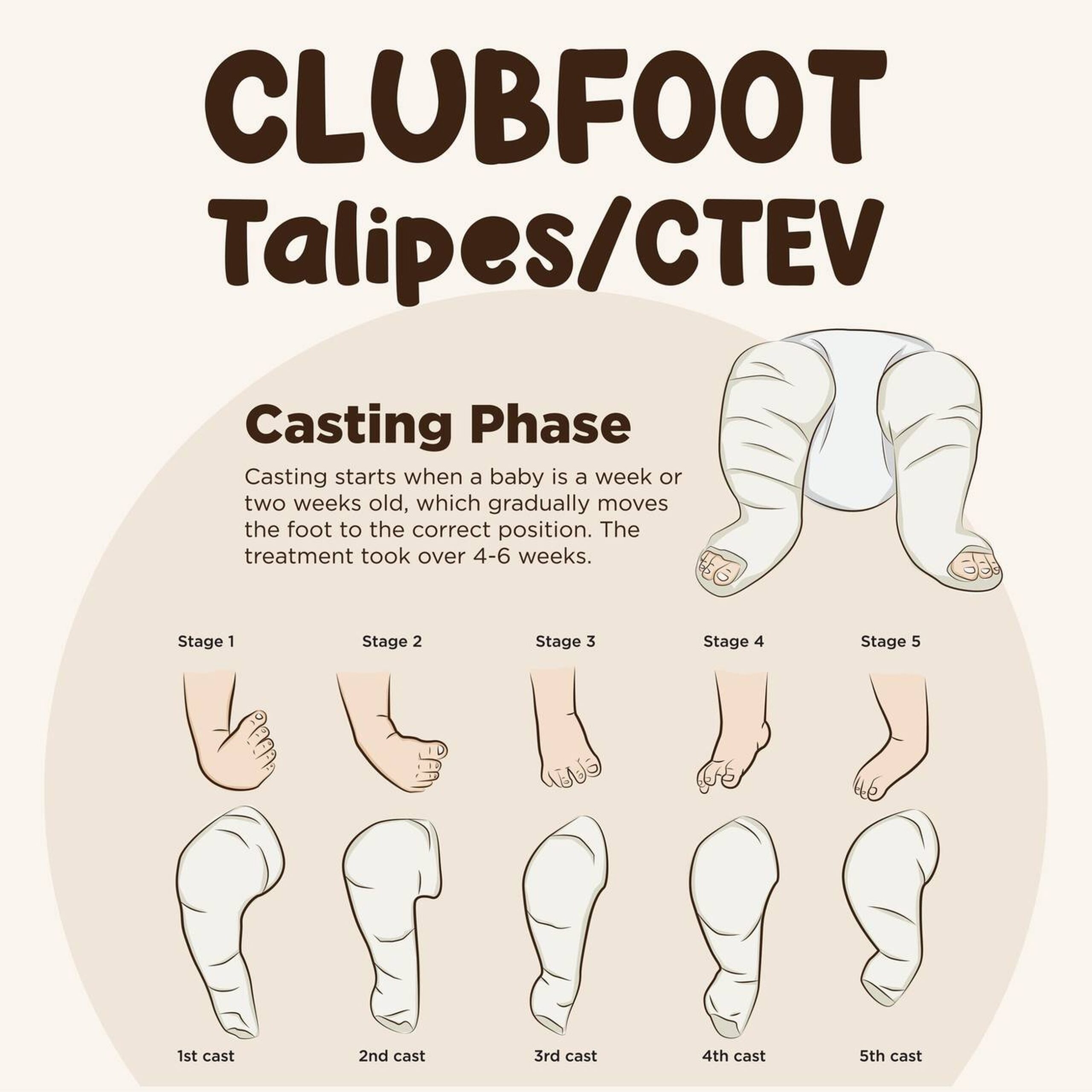
Clubfoot (Ponseti casting), metatarsus adductus, flatfoot, in‑toeing/out‑toeing, tarsal coalitions (older kids).
Gait concerns
In‑toeing, tip‑toe walking, knock‑knees, bow‑legs—assessment to distinguish normal variation from pathology.
Limb length & deformity
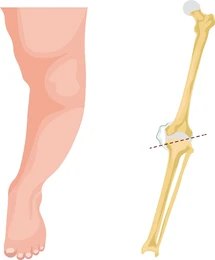
Length discrepancy, angular deformities around the knee/ankle; guided growth or osteotomy when indicated.
Paediatric fractures
Growth‑plate injuries, forearm fractures, supracondylar humerus—casting or pinning as needed.
Hip disorders (older kids)
Perthes disease, Slipped Capital Femoral Epiphysis (SCFE)—early diagnosis and stabilisation are critical.
Neuromuscular
Cerebral palsy and other conditions—orthopaedic procedures to improve comfort and function (with external physio coordination).
Spine
Scoliosis/kyphosis screening, bracing, coordination with paediatric spine services where needed.
Adolescent sports
Ligament and meniscus injuries, osteochondritis dissecans, apophysitis (Sever’s/Osgood‑Schlatter), recurrent patellar dislocation.
We distinguish normal developmental variants from conditions that need treatment—so you can avoid unnecessary worry or delay.
Evaluation & Diagnosis
- History & exam: Birth history, milestones, footwear, sports load; focused tests for hips, feet, gait, and alignment.
- Imaging: Ultrasound for infant hips; X‑rays for alignment or fracture; MRI selectively (e.g., cartilage/ligament issues).
- Growth‑aware reading: Age‑matched angles and lines—what looks “abnormal” in adults may be normal in kids.
- Shared plan: Clear discussion of options, timelines, benefits/risks, and how we measure progress.
We keep radiation exposure as low as reasonably achievable (ALARA) and use ultrasound or MRI when appropriate.

Non‑Surgical Care & External Physiotherapy
Many paediatric conditions improve with time and simple measures. We prefer observation, stretching, activity guidance, and bracing/casting when helpful. We do not provide in‑house physiotherapy. Instead, we share written, phase‑based protocols and coordinate with your physiotherapist or recommend external partners as needed.
Observation & guidance
Monitoring of physiologic bow‑legs/knock‑knees, flexible flatfeet, and gait variants that resolve with growth.
Casting & bracing
Ponseti casting for clubfoot, Pavlik harness for DDH (early), and corrective bracing where indicated.
Home exercise plans
Age‑appropriate stretches and strengthening with posture and balance cues (shared with your physio).
Activity & load advice
Modify sports load, training surfaces, and footwear to reduce pain and speed recovery.
Surgical Procedures (When Needed)
Clubfoot (Ponseti & tenotomy)
Most cases correct with serial Ponseti casts and a brief Achilles tenotomy; bracing follows to prevent recurrence.
DDH (hip reduction)
Closed reduction with spica casting when appropriate; open reduction / pelvic/femoral osteotomy for unstable or late‑presenting hips.
Guided growth (hemiepiphysiodesis)
Temporary plates guide growth to correct angular deformities with small incisions and minimal downtime.
Fracture fixation
Smooth/wire pinning for supracondylar humerus; flexible nails/plates for other fractures—growth plate protection is key.
SCFE stabilisation
Urgent in‑situ pinning for unstable slips; contralateral prophylaxis considered case‑by‑case.
Perthes & OCD procedures
Containment osteotomy (select Perthes); drilling or fixation for osteochondritis dissecans in appropriate lesions.
We aim for durable correction with the least disruption to growth and daily life.
Growth Plate & Alignment
Growth plates (physes) are the engines of limb length and alignment. Injuries or disease around physes can cause angular deformities or length differences. Early recognition and simple interventions can prevent bigger surgeries later.
- Guided growth: Small plates temporarily tether one side of a physis to straighten an axis as the child grows.
- Timing matters: We calculate remaining growth and choose the right window for correction.
- Osteotomy: For older children or severe deformity, precise bone cuts realign the limb.
Children’s Sports Injuries
Overuse and growth‑related injuries are common in active kids. We separate conditions that need rest and load changes from those that need bracing or surgery. Return‑to‑play is based on symptoms, strength, movement quality, and—when applicable—age‑appropriate criteria (not just the calendar).
Apophysitis
Sever’s disease (heel), Osgood‑Schlatter (knee)—load management, footwear, stretches, and external physio.
Patellar instability
First‑time dislocation often braced; recurrent cases may need MPFL reconstruction with growth‑friendly techniques.
ACL/meniscus (teens)
Growth‑sparing ACL approaches when indicated; meniscus repair preferred where feasible.
Anaesthesia, Imaging & Safety
- Child‑specific anaesthesia: Paediatric anaesthetists tailor sedation and pain control.
- Low‑dose imaging: ALARA principles; ultrasound/MRI when suitable; shielding and positioning to reduce exposure.
- Pain control: Child‑appropriate medications; nerve blocks when beneficial; clear home advice.
- Brace/cast care: Written do’s and don’ts to avoid skin issues and maintain correction.

Recovery & Follow‑Up
- Week 0–2: Swelling/pain control; cast/brace checks; gentle movement where safe.
- Week 3–6: Protected activity; school modifications; begin phase‑based external physio if required.
- Week 6–12: Strength, balance, and gait retraining; gradual return to sports skills.
- 3–6+ months: Full return to play once criteria (strength/movement) are met.
We do not provide in‑house physiotherapy. A written protocol is provided and coordinated with your physiotherapist; referrals to external clinics are available.

Cost & Insurance
Costs vary with diagnosis and plan—e.g., clinic evaluation, imaging (ultrasound/X‑ray/MRI), casting/bracing, or surgery (clubfoot tenotomy, guided growth, fracture fixation, DDH reduction). Facility and anaesthesia fees, implants/braces, and follow‑ups affect the estimate. We verify benefits and provide a transparent cost breakdown before scheduling your Paediatric Orthopaedics in Delhi treatment.
- Insurance pre‑authorisation & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

How to Prepare
Bring records
Pregnancy/birth details (for infants), prior clinic notes, imaging reports, school/sports letters.
Clothing & footwear
Loose clothes for cast/brace checks; bring usual shoes/sports footwear.
Comfort items
Snacks/water, a favourite toy or book—visits feel shorter with familiar comforts.
Questions & goals
Note your concerns: pain, limping, sport timelines, or school accommodations.
Plan for imaging
Some visits may require ultrasound/X‑rays—siblings and caregivers help keep little ones relaxed.
Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91-9810117204 to confirm.
Frequently Asked Questions
Is in‑toeing or flatfoot always abnormal?
When is surgery needed for DDH or clubfoot?
How do you decide on guided growth?
Do you provide physiotherapy?
How soon can my child return to sports?
Ready to help your child move with confidence?
Let’s design a child‑friendly plan tailored to your family’s goals.
