Scoliosis and Spine Deformity Surgery in Delhi
Scoliosis and Spine Deformity Surgery in Delhi offers comprehensive evaluation, bracing guidance, and surgical correction where indicated. We focus on precise diagnosis, growth‑aware planning for children and adolescents, and alignment‑restoring procedures for adults—backed by neuromonitoring, infection prevention, and enhanced recovery protocols. We do not provide in‑house physiotherapy; we share written protocols and coordinate with your physiotherapist for safe, criteria‑based rehabilitation.
Evaluation & imaging • Bracing • Posterior spinal fusion • Osteotomies • Neuromonitoring • Adult deformity correction. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)
About Scoliosis and Spine Deformity Surgery in Delhi
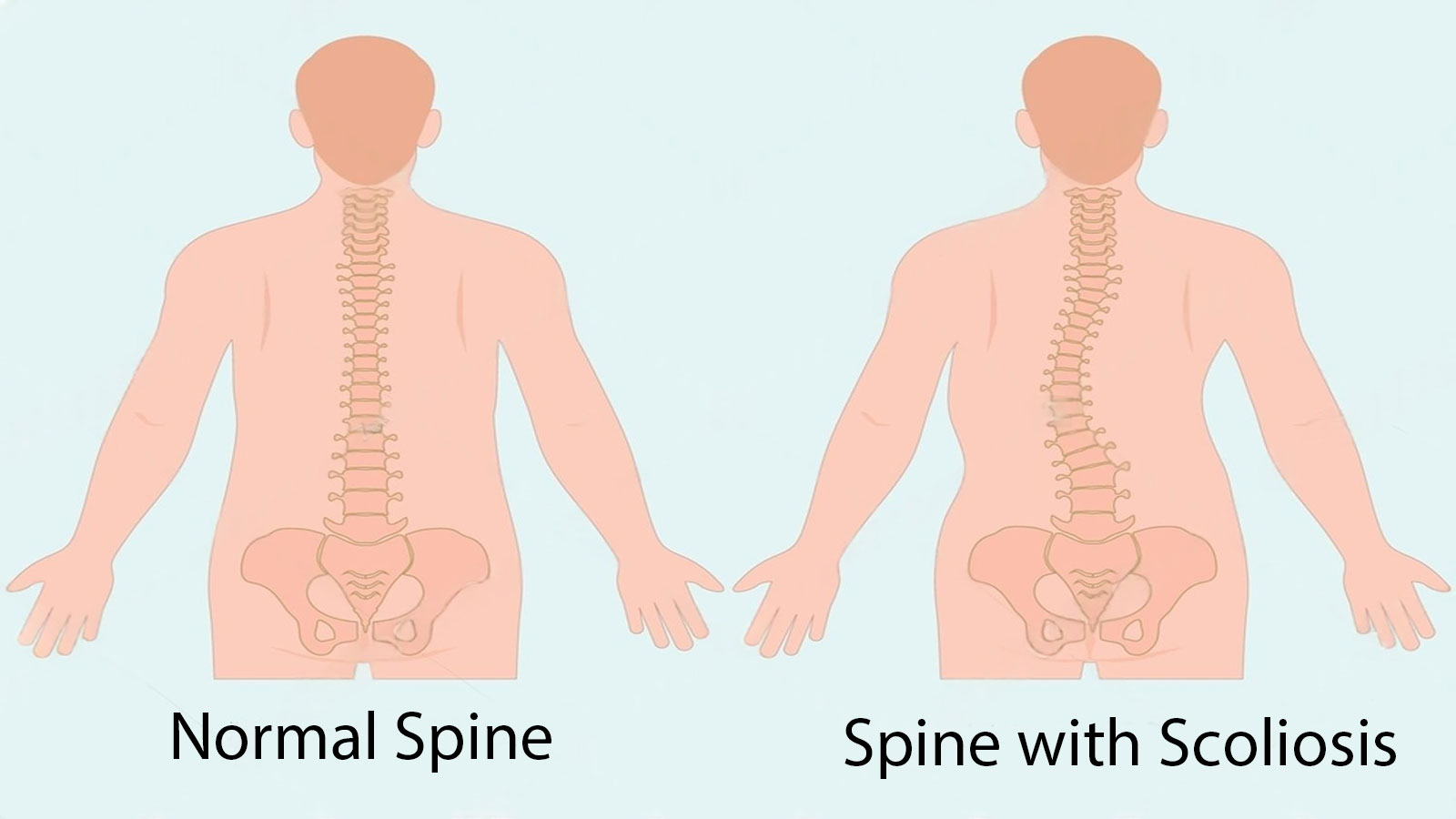
Scoliosis describes a three‑dimensional curvature of the spine that can occur in childhood (adolescent idiopathic scoliosis—AIS), from congenital vertebral anomalies, in neuromuscular conditions, or as adult degenerative deformity. Kyphosis (excess forward bend) and combined deformities also affect posture, comfort, and pulmonary function. Most curves are mild and simply monitored; some benefit from bracing during growth; a smaller subset needs surgery to prevent progression and restore balance.
Our program spans the full pathway—accurate measurement, growth assessment, bracing when indicated, and surgical correction when necessary. We emphasize safe alignment goals that respect the coronal (side‑to‑side) and sagittal (front‑to‑back) profile, because long‑term comfort depends on both. As Orthopedic Surgeons, we lead decision‑making on brace candidacy, fusion levels, osteotomy type, and implant strategy, coordinating with anesthesia, neuromonitoring, and pediatrics/medicine as needed.

Who It’s For & Types of Deformity
Adolescent idiopathic scoliosis (AIS)
Common in teens. Many curves remain mild; monitor if <30°. Consider bracing for 25–40° curves with growth remaining. Surgery typically considered at ≥45–50° or documented progression despite bracing.
Congenital scoliosis
Due to vertebral formation/segmentation defects; may progress quickly. Early imaging and tailored correction are critical; some require hemivertebra excision or growth‑friendly constructs.
Neuromuscular curves
Associated with cerebral palsy, muscular dystrophy, etc. Goals focus on seating balance, skin care, and caregiver ease, with multi‑disciplinary planning.
Adult degenerative deformity
Back/leg pain, stenosis, and imbalance from disc and facet degeneration. Options range from targeted decompression to short or long instrumented fusion based on symptoms and balance parameters.
Indications for surgery include progressive curves, structural deformity causing pain or imbalance, neurological compromise, or cardiopulmonary impact. Bracing has no role for established adult deformity but helps selected adolescents during growth.
Evaluation & Imaging
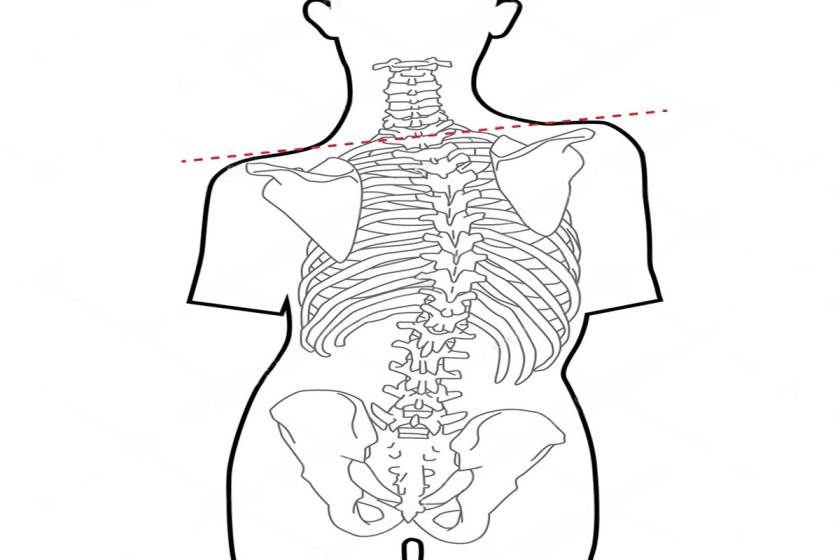
- History & exam: Growth status, pain pattern, neuro exam; scoliometer screening for rotation; shoulder/pelvic balance and sagittal profile.
- Standing X‑rays: Full‑length AP/lateral films (or EOS if available) to measure Cobb angles, coronal balance, pelvic parameters, and sagittal alignment.
- Flexibility studies: Side‑bending, traction, and prone films help decide fusion levels and need for osteotomies.
- MRI: For atypical curves, early onset, pain out of proportion, or neuro findings; screens for intraspinal anomalies (tethered cord, syrinx). For non‑deformity back/leg pain, see Sciatica & Back Pain Treatment in Delhi.
- CT (select cases): Useful in congenital anomalies to map pedicles and osteotomy planning.
- Risk work‑up: Pulmonary function tests for severe curves; bone health labs in adults; anesthetic risk stratification.
Clear radiographic and clinical correlation informs whether observation, bracing, or surgery is best.

Bracing: Indications & Protocols
Bracing aims to halt progression during growth; it does not “cure” scoliosis. We assess Risser/Sanders stage, curve magnitude, and pattern to guide brace candidacy and hours‑per‑day targets. We coordinate with certified orthotists, request in‑brace X‑rays to confirm correction, and adjust as the child grows. We do not provide physiotherapy in‑house; we share written protocols and work with your physiotherapist for scoliosis‑specific exercises where appropriate.
Who qualifies
AIS 25–40° with significant growth remaining. Good compliance (18–23 h/day) improves success.
Brace types
Boston/TLSO and Chêneau‑style braces are common; night‑time braces may suit select patterns.
Follow‑up
In‑brace film after 4–6 weeks; then out‑of‑brace films at regular intervals. Target ≥50% in‑brace correction for many patterns.

Surgical Planning & Techniques
When curves progress or cause symptoms, we plan surgery that achieves durable alignment while preserving as much mobility as possible. Our approach balances correction with safety, soft‑tissue respect, and long‑term spinal harmony. See also: Spinal Surgery in Delhi.
Posterior spinal fusion (PSF)
The mainstay for AIS and many adult deformities. Segmental pedicle screw constructs with rod derotation, translation, and compression/distraction maneuvers achieve three‑dimensional correction.
Osteotomies
Ponte/Smith‑Petersen osteotomies improve flexibility; pedicle subtraction osteotomy (PSO) or vertebral column resection (VCR) for severe rigid deformities in select cases.
Growth‑friendly options
For early‑onset scoliosis, growth‑friendly constructs may be considered to allow continued thoracic growth; candidacy is individualized.
Adult strategies
From decompression alone to limited fusion for segmental disease, up to full realignment for sagittal/coronal imbalance—guided by PI–LL targets and global balance. Bone health optimization reduces implant complications.
We set alignment goals that respect coronal balance and restore physiological lumbar lordosis and thoracic kyphosis for durable comfort.

Neuromonitoring & Safety
We use continuous intraoperative neuromonitoring—somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs)—to track spinal cord function during correction. Blood conservation (tranexamic acid, cell saver), meticulous hemostasis, and sterile technique reduce transfusions and infection risk. If signals change, corrective measures and a potential wake‑up test can be employed.
- Navigation/fluoroscopy: As indicated for pedicle screw accuracy in challenging anatomy.
- Infection prevention: Weight‑based antibiotics, layered closure, and negative‑pressure dressings for higher‑risk patients.
- VTE prevention: Early mobilization and risk‑adjusted prophylaxis.
For painful osteoporotic fractures (not deformity), see Vertebroplasty & Kyphoplasty.

Anesthesia & Pain Strategy
Balanced anesthesia supports stable neuromonitoring and smooth recovery. We use multimodal, opioid‑sparing analgesia, scheduled non‑opioids, antiemetic prophylaxis, and clear hydration/nutrition plans. In adults, we screen for sleep apnea and optimize comorbidities; in adolescents, we focus on early mobilization and sleep‑friendly pain regimens.
- Opioid‑sparing plan: Paracetamol and anti‑inflammatories when appropriate; adjuncts like gabapentinoids used selectively.
- Drain & catheter protocols: Streamlined to enable same‑day sitting/standing with the nurse team.
- Coordination: We do not provide physiotherapy in‑house; we supply written protocols and coordinate with your physiotherapist for safe progression.

Recovery & Follow‑Up
Most adolescents mobilize on day 1, climb stairs by day 2–3, and discharge by day 3–5 depending on pain and drains. Adults may require a slightly longer stay. We outline clear activity milestones and radiograph follow‑ups to ensure safe, steady progress. We do not provide physiotherapy in‑house; we supply written protocols and coordinate with your physiotherapist for posture training, safe transfers, and progressive conditioning.
- Week 0–2: Walk short distances daily; log‑roll technique for bed mobility; avoid bending/twisting/lifting >5 kg.
- Week 3–6: Increase walking tolerance; core engagement; wound review; school/desk work as tolerated for adolescents.
- Week 6–12: Gradual return to routine activities; light stretching; discuss driving/commute readiness.
- Beyond 3 months: Low‑impact sport progression; return to higher‑impact activities individualized after imaging and strength checks.
Follow‑up X‑rays typically at 6 weeks, 3 months, 6 months, and 1 year. We reinforce bone health, posture, and safe activity as the fusion matures.

Risks & Complications
Neurological injury
Uncommon with modern techniques and neuromonitoring; rapid recognition and correction protocols are in place.
Infection
Reduced by pre‑incision antibiotics, sterile technique, and wound care; higher‑risk patients may benefit from NPWT dressings.
Blood loss
Mitigated with tranexamic acid, cell saver, and meticulous technique.
Implant issues
PJK/adjacent segment disease, hardware failure, or pseudarthrosis can occur over time, especially with poor bone quality or smoking.
Medical risks
VTE, pulmonary, and anesthesia‑related risks are managed with multidisciplinary protocols and early mobilization.
Cost & Insurance
Costs depend on curve type and stiffness, number of levels, osteotomy complexity, implant choices, neuromonitoring/navigation needs, ICU stay, and total hospital days. Most insurers cover medically necessary scoliosis and deformity correction. We verify benefits and provide a transparent estimate before scheduling your Scoliosis and Spine Deformity Surgery in Delhi.
- Insurance pre‑authorization & benefits check
- Clear estimate of surgeon, hospital, anesthesia, and implant costs
- Cashless/financing options where applicable
How to Prepare
Records & imaging
Bring prior notes, standing full‑spine X‑rays, bending films, and any MRI/CT on CD. Growth records (height trends) help in AIS.
Medications
Share blood thinners and supplements; some require timed pauses. Manage diabetes/thyroid medicines per anesthetist guidance.
Bone health
Adults benefit from vitamin D optimization and bone‑strength planning to reduce implant complications.
Home setup
Arrange a firm chair with arms, raise frequently used items, and plan family support for the first two weeks.
Physio & orthotist
We do not provide physiotherapy in‑house; share your physiotherapist’s contact for protocol alignment. For bracing, bring your orthotist’s details.
Where to Consult Dr. Neelabh
BLK Hospital
A‑4‑6, Pusa Rd, Near Rajendra Place Metro, New Delhi‑110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91‑9810117204 to confirm.
FAQs
Do all scoliosis curves need surgery?
Will a brace straighten my spine permanently?
How long is hospital stay and recovery?
Is neuromonitoring used in all cases?
Do you provide physiotherapy?
Need Scoliosis and Spine Deformity Surgery in Delhi?
Book a consultation. We’ll clarify diagnosis, review bracing candidacy, and plan safe, durable correction when surgery is indicated.
