Foot and Ankle Surgery in Delhi
Foot and Ankle Surgery in Delhi covers bunion, flatfoot, ankle instability, Achilles problems, and ankle arthroscopy. We deliver reconstruction and arthroscopy for durable comfort and stability—personalized plans that start with precise diagnosis and conservative care, progressing to minimally invasive or open correction when required. We do not provide in‑house physiotherapy; we share written protocols and coordinate with your physiotherapist for criteria‑based rehab and safe return to activity.
Bunion • Flatfoot • Instability • Achilles • Arthroscopy • Fusion/realignment • Footwear & prevention. Serving patients across Delhi & NCR (Naraina, Karol Bagh, Patel Nagar, and more)
About Foot and Ankle Surgery in Delhi
Foot problems can make every step feel like work—painful big toe bunions, flatfoot collapse with fatigue, ankle “giving way,” heel pain, or deep ankle aches after a twist. Our program prioritizes clear diagnosis, conservative care, and minimally invasive techniques where appropriate. When surgery is indicated, we target root causes: alignment, ligament stability, tendon power, and joint cartilage health—to achieve durable comfort and confident mobility.
We integrate careful imaging with pragmatic decision‑making. As orthopedic surgeons, we lead choices on osteotomies, ligament reconstruction, tendon transfers, arthroscopy, and when necessary, fusion—coordinating with anesthesia, radiology, and your physiotherapist for a coherent plan from diagnosis to recovery.

Conditions We Treat
Bunion (Hallux Valgus)
Painful bump and toe drift; corrected with soft‑tissue balancing and osteotomy or TMT fusion depending on severity and instability.
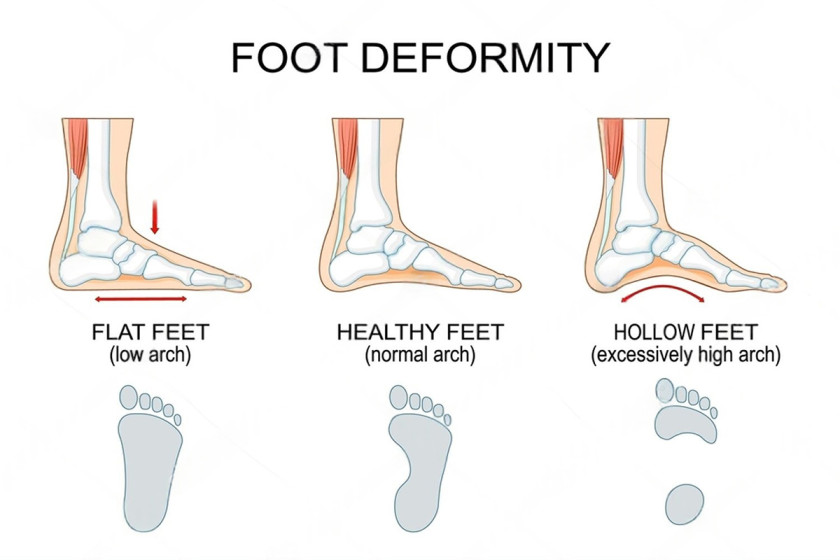
Flatfoot (Adult Acquired)
Posterior tibial tendon dysfunction (PTTD) with arch collapse, forefoot abduction, and heel valgus; staged reconstruction tailored to flexibility.
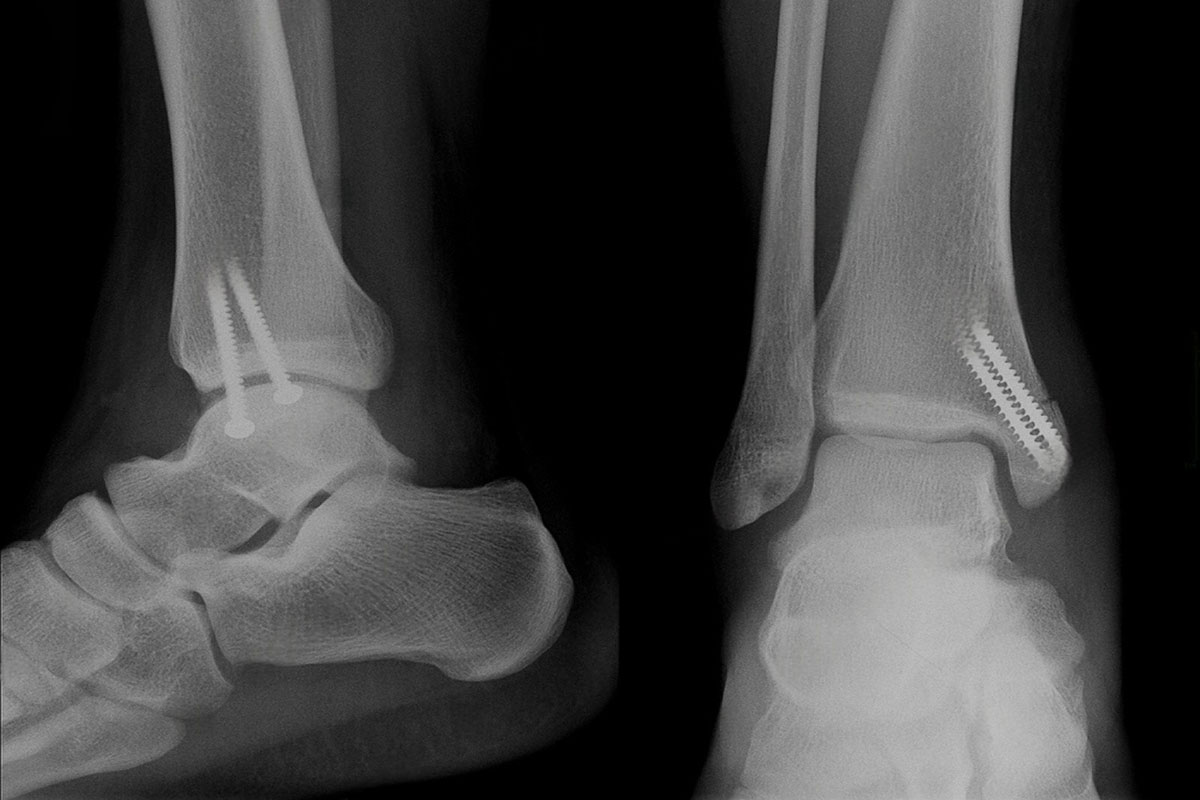
Chronic Ankle Instability
Repeated sprains, “giving way,” and swelling; Broström‑type repair ± internal brace for durable lateral stability.
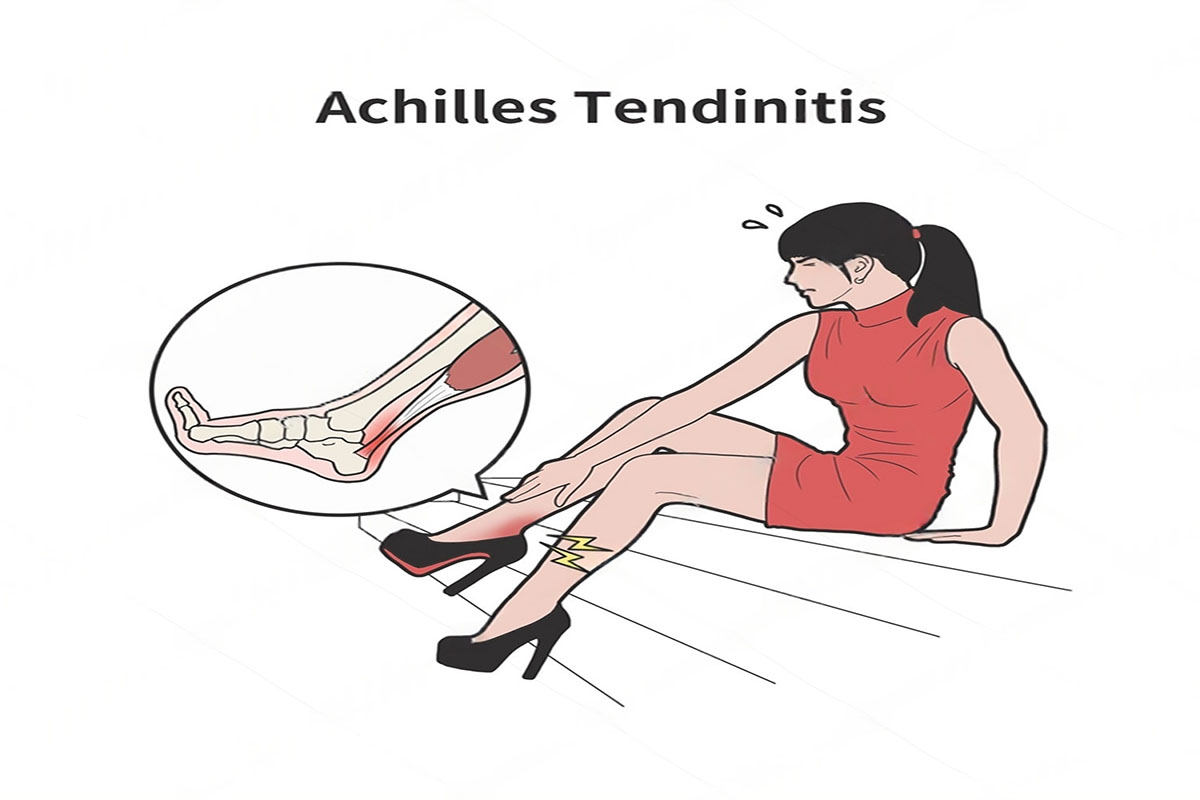
Achilles Disorders
Mid‑portion tendinopathy, insertional pain/Haglund’s, or rupture; options range from structured rehab to minimally invasive repair.
Ankle Impingement & OCL Talus
Front or back ankle pain, locking/catching; arthroscopy for debridement, microfracture, or grafting where indicated.
Arthritis & Deformity
Midfoot/hindfoot arthritis, cavovarus/planovalgus; realignment osteotomy or fusion for pain relief and plantigrade stance.
We also manage plantar fasciitis refractory to care, peroneal tendon issues, and selected sports injuries of the foot and ankle.
Evaluation & Imaging
- Clinical exam: Gait, hindfoot alignment, forefoot abduction, calf flexibility, ligament laxity (anterior drawer/talar tilt), and tenderness mapping.
- Weight‑bearing X‑rays: AP/lateral/oblique, hindfoot alignment view; hallux angles; Meary’s angle; talar uncoverage.
- MRI: PTT tears, spring ligament integrity, peroneals, osteochondral lesions of talus, and occult impingement.
- Ultrasound: Dynamic tendon evaluation (Achilles/peroneals) and guided injections.
- CT (select cases): 3D planning for deformity, end‑stage arthritis, or revision scenarios.
We line up your symptoms with imaging so treatment targets the true pain generator.
Conservative Care First
Most conditions improve with structured non‑operative care. We personalize a plan you can follow at home and at work. We do not provide physiotherapy services in‑house; we supply written protocols and coordinate with your physiotherapist.
Footwear & insoles
Wide toe box for bunions, rocker‑sole shoes for forefoot pain, medial posting for flatfoot, lateral posting for cavovarus.
Bracing
AFO or lace‑up brace for flatfoot/instability; night splints for plantar fasciitis; CAM boot for acute tendon irritability.
Exercise protocols
Eccentric calf loading, PTT strengthening, peroneal control, balance drills, plantar fascia stretches—progressed by criteria.
Injections
Ultrasound‑guided steroid for sinus tarsi or retrocalcaneal bursitis; judicious use around tendons; viscosupplement or PRP in select joints.
Surgery is reserved for persistent pain, recurrent instability, or deformity that blocks function.
Bunion & Forefoot Correction
Bunions form when the first metatarsal drifts medially and the big toe rotates/leans laterally, creating a painful prominence and shoe conflict. We match correction to deformity severity and joint stability.
Distal osteotomies
Chevron/scarf with soft‑tissue balancing for mild–moderate deformity; add Akin osteotomy for toe alignment.
Lapidus (first TMT fusion)
Best for hypermobility/instability or larger angles; stabilizes the base and improves long‑term alignment.
Lesser toe issues
Hammertoe correction, plantar plate repair, neuroma care, and tailored metatarsal procedures.

Weight‑bearing in a post‑op shoe is common after distal osteotomy; Lapidus procedures typically need protected weight‑bearing longer.
Flatfoot & PTTD Reconstruction
Adult acquired flatfoot (Stage II) is often a flexible deformity from posterior tibial tendon dysfunction and spring ligament attenuation. We combine procedures that correct hindfoot valgus, forefoot abduction, and medial column collapse.
- Medializing calcaneal osteotomy: Brings the heel under the leg for improved leverage.
- FDL transfer ± spring ligament repair: Restores medial support and tendon power.
- Lateral column lengthening (Evans): Corrects forefoot abduction in select patterns.
- First ray procedures: Cotton osteotomy or medial column fusion for persistent forefoot varus.
- Stage III/IV: Hindfoot/triple fusion and, when needed, ankle procedures for rigid deformity.
Expect a period of non‑weight‑bearing followed by progressive loading in a boot, guided by healing and alignment on X‑rays.

Ankle Instability Solutions
For recurrent sprains or a chronically weak ankle, we repair or reconstruct lateral ligaments and address associated issues (peroneal tendons, bony impingement, os subfibulare). Many patients come with recurrent ankle sprain that never fully recovered, leading to chronic instability.
- Broström‑Gould repair: Capsuloligamentous repair of ATFL/CFL; add internal brace augmentation for early stability in selected patients.
- Peroneal procedures: Debridement/repair, retinaculum repair; groove deepening when indicated.
- Alignment adjuncts: Varus hindfoot may need corrective osteotomy to protect the repair.
Most patients transition from boot to brace by 4–6 weeks and return to sport‑specific drills around 10–12 weeks with criteria‑based progression.

Achilles Tendon: Rupture & Tendinopathy
We treat Achilles problems with the least invasive option that restores power safely. Acute ruptures can be managed operatively or non‑operatively depending on gap, demands, and timing. Tendinopathy care emphasizes load management and calf remodeling.
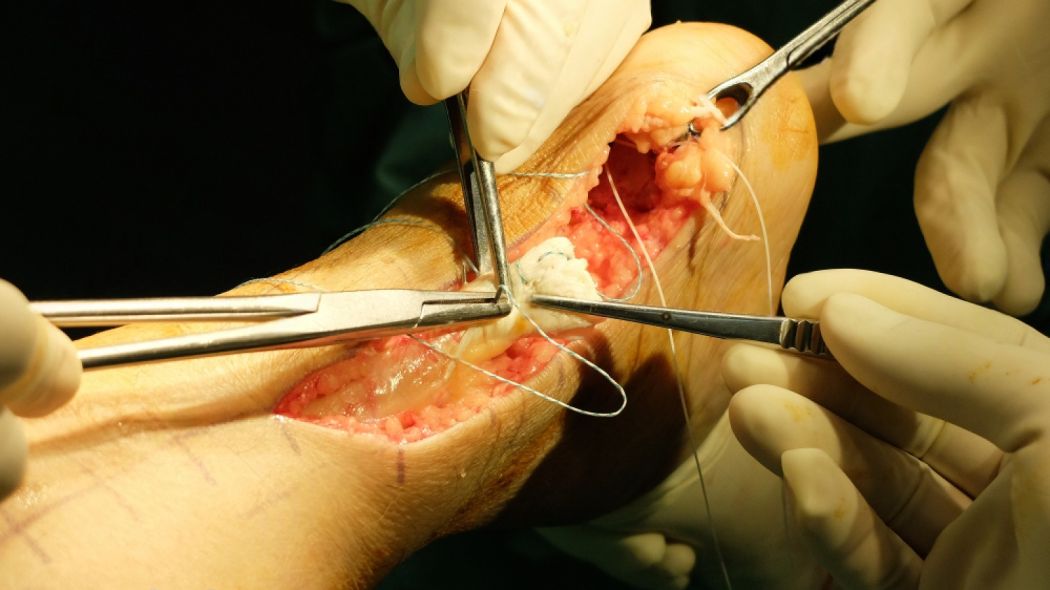
Rupture repair
Mini‑open/percutaneous repair with functional rehab pathways; non‑operative functional bracing for select, timely cases.
Insertional disease
Debridement, Haglund’s resection, and calcific spur management; FHL transfer when tissue quality is poor.
Mid‑portion tendinopathy
Eccentric loading, shockwave, or limited debridement; ultrasound‑guided interventions as needed.
Ankle Arthroscopy & Cartilage Lesions
Arthroscopy helps diagnose and treat impingement, synovitis, loose bodies, and cartilage injuries with minimal soft‑tissue disruption.
- Impingement debridement: Anterior/posterior impingement relief to restore painless motion.
- OCL talus: Microfracture or drilling for smaller contained lesions; grafting or OATS in select cases; adjunct biologics considered.
- Synovectomy & loose body removal: For clicking, locking, or recurrent swelling.
Most arthroscopy patients walk in a boot early and progress activity over 4–8 weeks.
Arthritis: Fusion & Alignment
For painful midfoot or hindfoot arthritis and severe deformity, fusion restores a stable, plantigrade foot. In ankle arthritis, options include arthroscopic debridement (early) or ankle fusion; ankle replacement may suit select patients after candidacy review.
Midfoot/hindfoot fusion
Targeted or multi‑joint fusion based on pain pattern; alignment is set to optimize walking and shoe wear.
Ankle fusion
For end‑stage arthritis with deformity; stable pain relief with gait adaptations and rocker‑sole footwear.
Adjunct procedures
Gastrocnemius recession, osteotomies, or tendon balancing to protect the reconstruction.

Anesthesia & Pain Strategy
We favor regional anesthesia (popliteal/saphenous blocks) with light sedation and a multimodal, opioid‑sparing plan. Simple dosing schedules and night‑time comfort measures support early mobilization and good sleep.
- Regional blocks: Reduce nausea and improve early pain control, especially after osteotomies or fusion.
- Opioid‑sparing: Acetaminophen ± anti‑inflammatories when appropriate; gastric/renal precautions individualized.
- Coordination: We do not provide physiotherapy in‑house; we supply written protocols and coordinate with your physiotherapist.

Recovery & Rehabilitation
We provide a written, procedure‑specific plan and coordinate with your physiotherapist; we do not provide physiotherapy in‑house. Weight‑bearing and activity depend on the operation and bone/soft‑tissue quality.
- Bunion osteotomy: Post‑op shoe; heel weight‑bearing immediately or as advised; swelling settles over weeks.
- Lapidus/flatfoot reconstruction: 4–6 weeks non‑weight‑bearing, then progressive loading in a boot by X‑ray criteria.
- Broström repair: Boot 2–4 weeks then brace; balance/strength progression; jog drills by ~10–12 weeks.
- Achilles repair: Protected plantarflexion, staged ROM, and criteria‑based strengthening; running progression typically 3–4 months.
- Arthroscopy (impingement/OCL): Early ROM; impact and pivoting restricted until strength and comfort allow.
- Fusions: Longer protection; shoe modifications and orthoses improve comfort during gait retraining.
Milestones include swelling control, wound healing, symmetric step length, single‑leg balance, and pain‑free push‑off.

Footwear, Orthoses & Prevention
Footwear
Roomy toe box for bunions, rocker‑sole for forefoot arthritis, cushioned heels for Achilles/insertional pain.
Insoles/orthoses
Medial arch support for flatfoot, lateral posting for varus, met pads for forefoot off‑load.
Activity & strength
Regular calf/foot intrinsic work, balance drills, and gradual mileage increases to prevent recurrence.
Simple shoe and insole choices often make the biggest difference day‑to‑day.
Risks & Safety
Infection & wound issues
Reduced by sterile technique, elevation, and careful dressing; higher risk with smoking/diabetes.
Nerve sensitivity/numbness
Usually improves with time; scar care helps.
Nonunion/hardware irritation
Rare with modern techniques; may need protection or later hardware removal.
DVT
Risk‑stratified prophylaxis and early ankle motion reduce risk.
Residual symptoms
Under‑/over‑correction or arthritis progression can occur; we plan to minimize these upfront.
Cost & Insurance
Costs depend on diagnosis (bunion vs flatfoot vs instability vs fusion), implants (screws/plates/anchors), anesthesia type, length of stay, and imaging needs. Many procedures are day‑care; reconstructions may need an overnight. Most insurers cover medically necessary Foot and Ankle Surgery. We verify benefits and provide a transparent estimate before scheduling your Foot and Ankle Surgery in Delhi.
- Insurance pre‑authorization & benefits check
- Clear estimate of surgeon, hospital, anesthesia, and implant costs
- Cashless/financing options where applicable

How to Prepare
Records & imaging
Bring previous notes, weight‑bearing X‑rays, any MRI/ultrasound, and shoes/orthoses you currently use.
Medications
Share blood thinners/diabetes meds; some require timed pauses. Ask about fasting if sedation is planned.
Home setup
Arrange crutches/boot, clear walkways, organize help for the first week after reconstruction.
Smoking & sugars
Stop nicotine; optimize glucose—both are critical for wound healing and bone union.
Physiotherapist contact
We do not provide physiotherapy in‑house; share your physiotherapist’s details so we can align written protocols.
Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91‑9810117204 to confirm.
FAQs
Do all bunions need surgery?
How long will I be off my feet after flatfoot reconstruction?
When can I return to sport after ankle ligament repair?
Is arthroscopy always the answer for ankle pain?
Do you provide physiotherapy?
Need Foot and Ankle Surgery in Delhi?
Book a consultation. We’ll confirm your diagnosis, outline conservative options, and plan precise reconstruction or arthroscopy for durable comfort and stability.
