ACL Reconstruction in Delhi (Ligament Reconstruction)
ACL Reconstruction in Delhi with Dr. Neelabh uses arthroscopic keyhole techniques, anatomic graft placement, and modern fixation to restore knee stability for sport and daily life.
Keyhole surgery • Anatomic grafts • Clear rehab protocol (with your physiotherapist)
Keyhole precision
Arthroscopic approach with HD optics for anatomic tunnel placement and stable fixation.
Graft options
Hamstring, quadriceps tendon, or BPTB—recommended to match your sport and anatomy.
Sport-ready plan
Clear, criteria‑based return‑to‑sport roadmap your physiotherapist can follow.
Honest guidance
We don’t provide in‑house physiotherapy; we coordinate with your chosen therapist and supply written protocols.
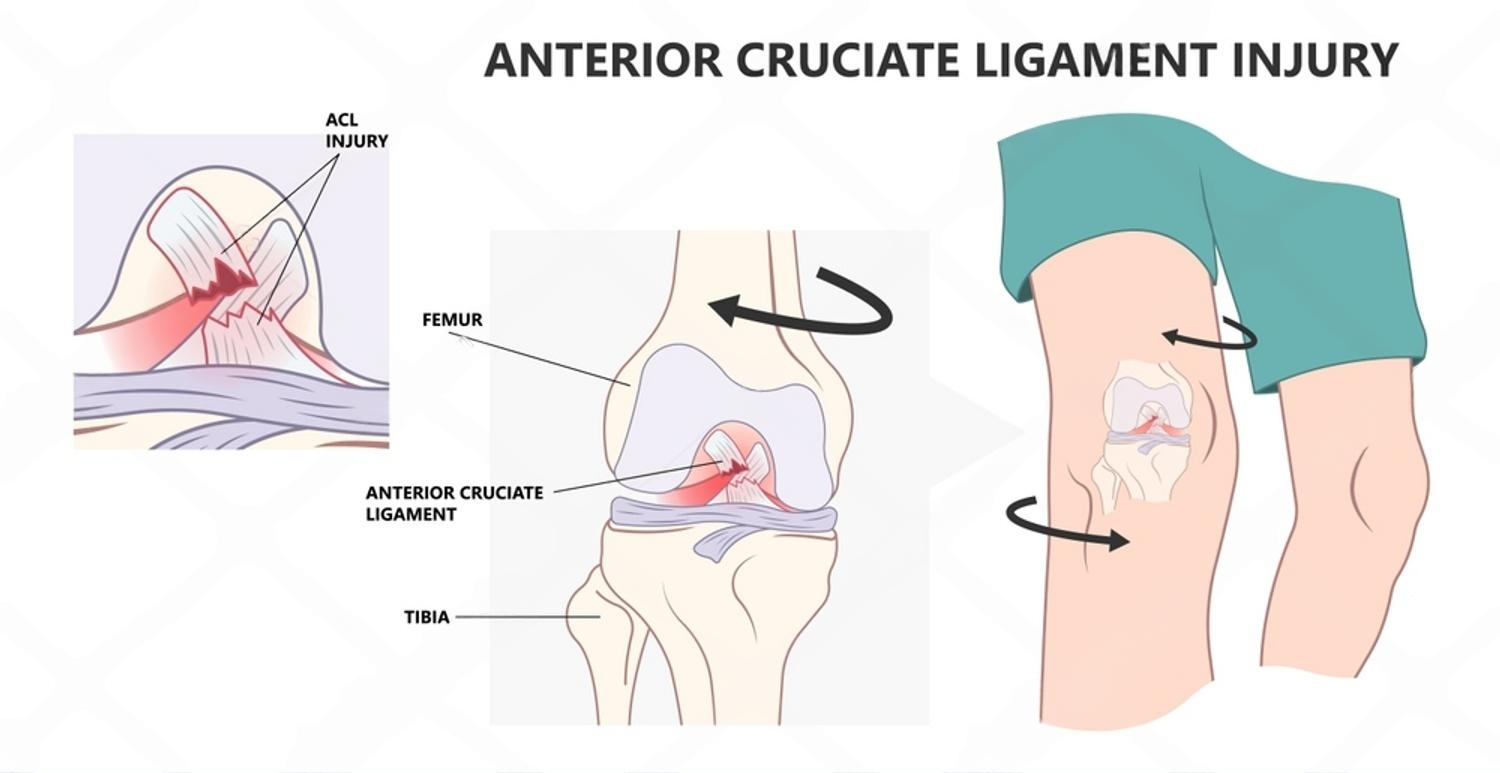
What is ACL Reconstruction in Delhi?
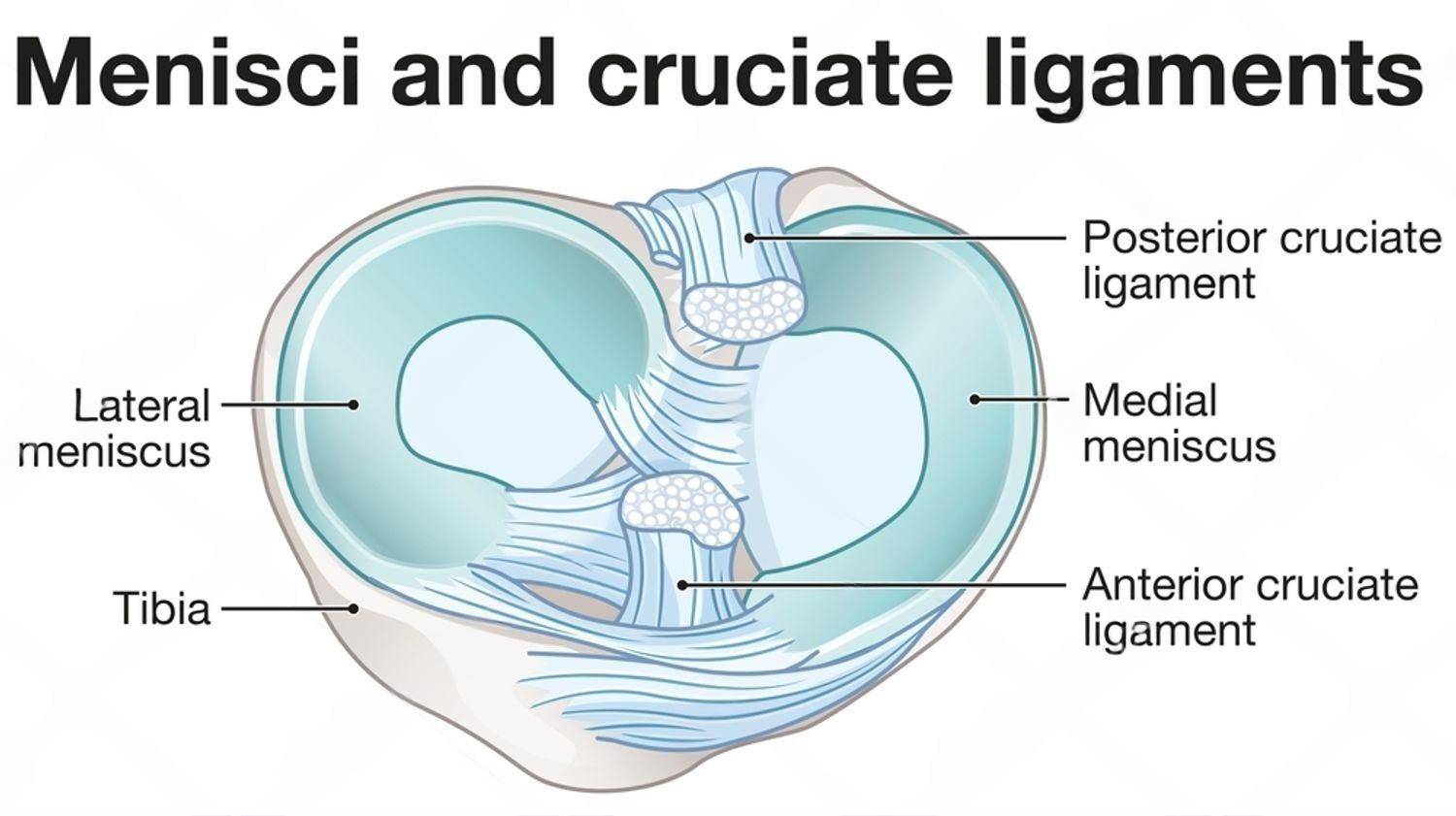
ACL/Ligament Reconstruction restores stability to a knee that “gives way” after injury. Using arthroscopy, tunnels are created in the femur and tibia to place a tendon graft that functions like your original ACL. Associated meniscus or cartilage injuries can be treated in the same sitting.
Other ligament injuries (PCL, MCL, LCL, PLC) may require reconstruction or augmentation depending on instability and sport demands.

Who Needs ACL / Ligament Reconstruction?
Instability with pivoting
Knee “giving way” during turns, jumps, or uneven ground.
Active lifestyle
Return to pivoting sports (football, basketball, badminton) or manual work.
Associated injuries
Meniscus tears, cartilage damage, or multi‑ligament injuries.
Failed conservative care
Persistent instability despite bracing and targeted exercises.
Patients seeking ACL Reconstruction in Delhi receive an honest assessment and a tailored surgical + rehab plan.
Graft Choices
- Hamstring (STG): Popular, strong, low kneeling pain; size matters for strength.
- Quadriceps tendon: Excellent strength; useful if hamstrings are small or revision cases.
- BPTB (Bone‑Patellar Tendon‑Bone): Rigid fixation; more anterior knee/kneeling pain risk.
- Allograft: Considered in select revisions or multi‑ligament cases.
We’ll discuss pros/cons based on age, sport, anatomy, and goals.
Benefits
- Improved knee stability and confidence
- Protection of meniscus and cartilage with stable mechanics
- Return to sport and active work with criteria‑based progression
- Arthroscopic keyhole approach with small incisions
Risks & How We Reduce Them
- Infection, clots, stiffness—reduced with protocols and early guided motion
- Re‑tear or laxity—minimised by anatomic tunnels and strong fixation
- Kneeling/anterior knee pain—discussed when choosing graft type
How ACL Surgery is Performed
- Anaesthesia & positioning: Regional or general anaesthesia; careful positioning and sterile prep.
- Arthroscopy & assessment: Joint inspected; meniscus/cartilage treated as indicated.
- Graft harvest & prep: Hamstring, quadriceps, or BPTB prepared to target diameter/length.
- Tunnels & fixation: Anatomic femoral/tibial tunnels drilled; graft fixed with buttons/screws.
- Closure & bracing: Small sutures; brace and immediate post‑op instructions provided.
Meniscus‑first approach
Repairs performed when possible to protect long‑term joint health.
Multi‑ligament strategy
Staged or combined procedures for PCL/MCL/LCL/PLC as needed.
Bracing & protocols
You’ll receive a written rehab pathway your physiotherapist can follow.
Recovery & Return to Sport
- Week 0–2: Swelling control, heel slides, quadriceps sets; brace/crutches as advised.
- Week 3–6: Gradual range‑of‑motion and early strength; normal gait training.
- Week 6–12: Progressive strengthening and controlled drills; light cycling/elliptical.
- Month 4–6+: Plyometrics, agility, sport‑specific work; return to play when criteria met.
Note: We don’t provide in‑house physiotherapy. We supply protocols and coordinate with your chosen physiotherapist (or can recommend external options).

Cost & Insurance
Costs vary by graft choice, fixation implants, facility and anaesthesia fees, and coverage. We verify benefits and provide a transparent estimate before scheduling your ACL Reconstruction in Delhi.
- Insurance pre‑authorisation & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91-9810117204 to confirm.
How to Prepare
Medical clearance
Pre‑op evaluation, labs, ECG, and imaging as needed.
Medication review
Guidance on blood thinners, diabetes medicines, and supplements.
Prehab (external)
We recommend prehab with your physiotherapist: swelling control, quad activation, full extension.
Home setup
Ice, brace, safe pathways, and support for initial days.
Nutrition & habits
Stop smoking, optimise blood sugar, hydrate, and prioritise protein.
Frequently Asked Questions
Do I need surgery for a torn ACL?
Which graft is best?
Is it day‑care surgery?
When can I walk or climb stairs?
Do you provide physiotherapy?
When can I return to sport?
Ready to stabilise your knee?
Let’s build a surgical and rehab plan that matches your sport and goals.
