Arthritis & Rheumatology Care in Delhi
Arthritis & Rheumatology Care in Delhi with Dr. Neelabh focuses on accurate diagnosis, personalized medical therapy, non‑PRP injection options, bracing/orthotics, and clear guidance on when joint preservation or replacement is best. We do not provide in‑house physiotherapy; we share written home‑exercise protocols and coordinate with your chosen physiotherapist.
Evidence‑based medicine • Treat‑to‑target • Safety monitoring • Surgical options when needed
About Arthritis & Rheumatology
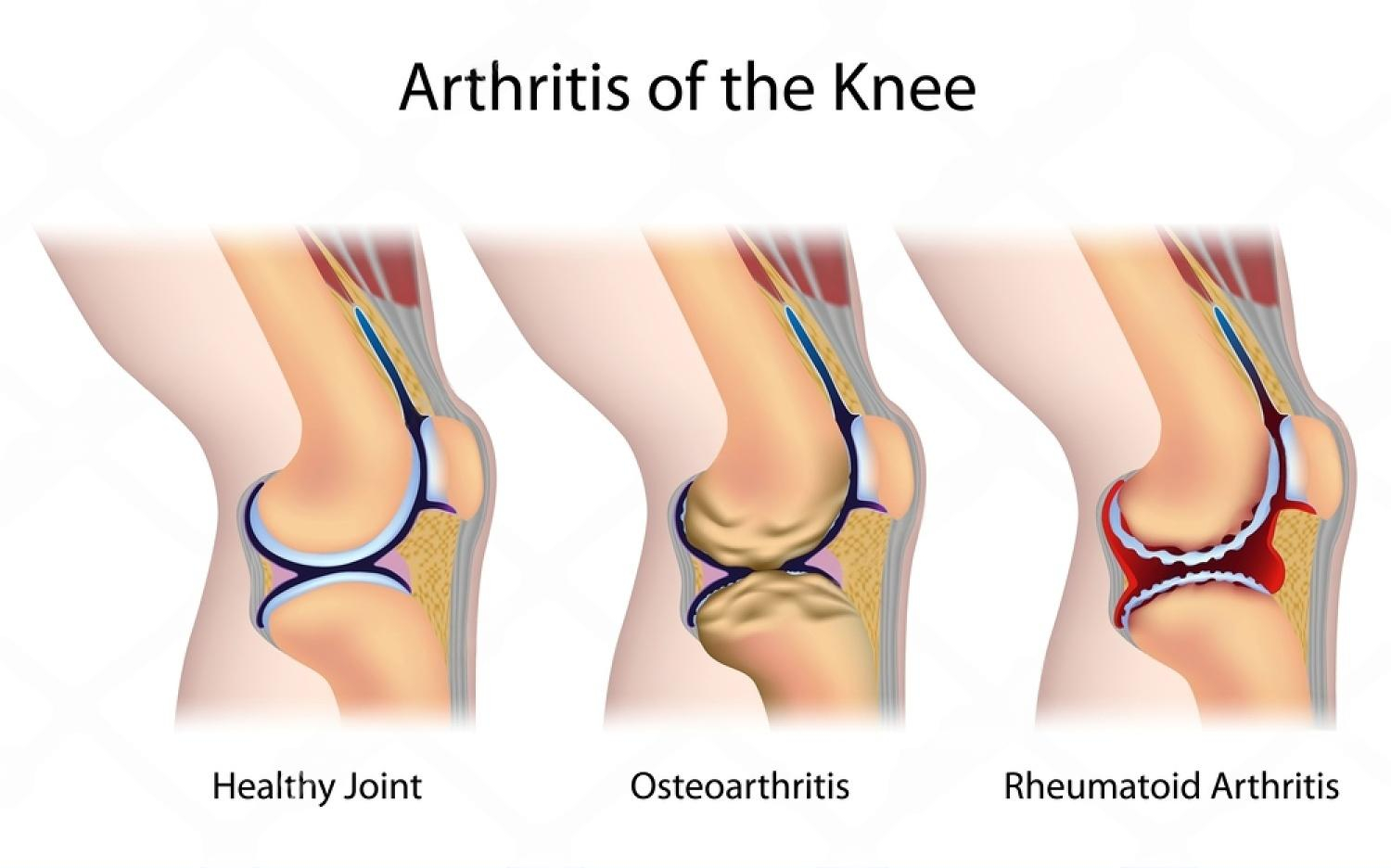
“Arthritis” covers many conditions that cause joint pain, stiffness, swelling, and reduced function. Broadly, we see two groups: degenerative arthritis (such as osteoarthritis) where cartilage gradually wears down, and inflammatory arthritis (such as rheumatoid arthritis, psoriatic arthritis, and spondyloarthritis) where the immune system drives joint inflammation and tissue damage. A third group includes crystal arthritis (gout and calcium pyrophosphate deposition disease), connective tissue diseases (lupus), and infection‑related arthritis.
Our goal is to pinpoint the cause and stage of your condition and match it with the least‑invasive, most effective plan. That often includes education, lifestyle measures, appropriate medicines, targeted injections when indicated, and—only when necessary—surgical options such as joint preservation osteotomies or joint replacement. Throughout, we keep the focus on pain control, function, safety, and your personal goals for work and life.
Symptoms & When to Seek Care
Osteoarthritis (OA)
Deep ache, stiffness after rest, creaking (crepitus), swelling after activity, reduced range of motion—common in knees, hips, hands.
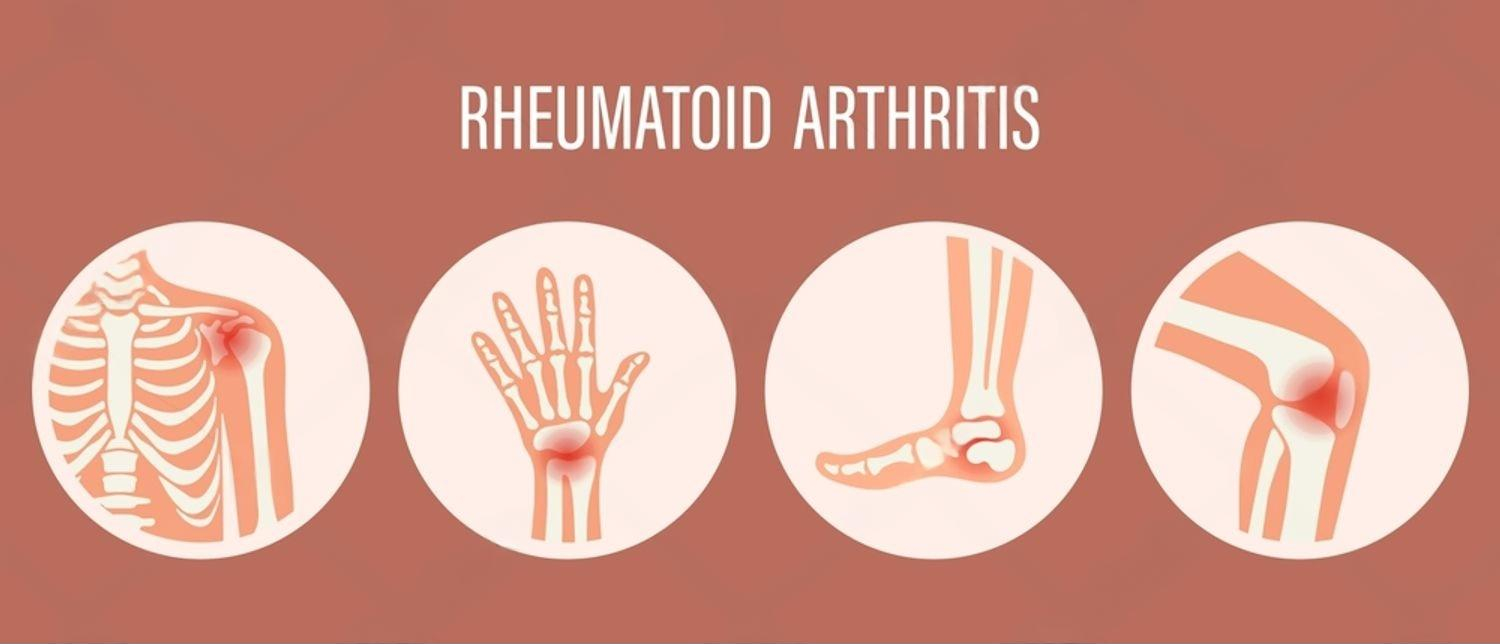
Rheumatoid arthritis (RA)
Morning stiffness >30–60 minutes, small‑joint swelling in hands/feet, fatigue; symptoms improve with movement.
Spondyloarthritis
Back pain that improves with exercise (not rest), heel pain, or swollen fingers/toes; link with psoriasis, uveitis, or bowel disease.
Gout/CPPD
Sudden red, hot, swollen joint (often big toe, ankle, knee); flares triggered by diet, dehydration, or illness.
Red flags (seek urgent care): fever with a hot swollen joint, inability to bear weight, new weakness or numbness, or severe night pain with weight loss.
Evaluation & Diagnosis
- Clinical assessment: Joint exam, function, gait, and history including family predisposition, infections, skin/nail changes, eye or bowel symptoms.
- Imaging: X‑rays for alignment, joint space and osteophytes; ultrasound to detect synovitis/effusion; MRI for early cartilage/bone marrow inflammation when needed.
- Lab tests: ESR/CRP (inflammation), RF and anti‑CCP (RA), HLA‑B27 (spondyloarthritis), uric acid (gout), ANA (connective tissue disease), and others tailored to history.
- Joint fluid analysis: Confirms crystal arthritis (gout/CPPD) or rules out infection before steroid injection.
- Risk review: Comorbidities (diabetes, hypertension, liver/kidney disease), medication interactions, and vaccination status prior to biologics.
Diagnosis is not just a label—it guides the plan. For inflammatory arthritis, we use treat‑to‑target strategies to control inflammation and protect joints. For osteoarthritis, we combine lifestyle measures, medications, bracing/orthotics, and procedural options to manage pain and preserve function.

Treatment Plan (Medical & Lifestyle)
Education & daily habits
Weight management for knee/hip OA; pacing activities; joint‑friendly movement; sleep and stress strategies. We provide written guidance and coordinate with your physiotherapist for a home‑exercise plan—no in‑house physiotherapy provided.
Osteoarthritis medicines
Topical NSAIDs, acetaminophen, oral NSAIDs (case‑by‑case), duloxetine, and short courses of pain modulators where appropriate. For hand OA, splints and topical agents often help; for knee OA, injections may be considered.
Inflammatory arthritis therapy
For RA/psoriatic arthritis/spondyloarthritis: conventional DMARDs (methotrexate, leflunomide, sulfasalazine, hydroxychloroquine), biologic agents (TNF‑α/IL‑6/IL‑17 inhibitors, abatacept) or targeted synthetic DMARDs (JAK inhibitors). We screen for TB/hepatitis where required and monitor labs.
Crystal arthritis (gout/CPPD)
Flare control: colchicine, NSAIDs, or short steroid taper (if appropriate). Prevention: urate‑lowering therapy (allopurinol/febuxostat) with gradual titration to target urate, plus diet/hydration guidance.
Comprehensive safety
Medication interactions, BP/glucose checks with steroids or NSAIDs, liver/kidney monitoring, and vaccination planning with immunomodulators.
We focus on the least‑invasive plan that controls symptoms and protects joint health. If pain or inflammation remains despite best medical care, we discuss procedural and surgical options.
Non‑PRP Injection Therapies
In selected cases, targeted injections offer meaningful relief while you continue core therapies. We do not offer PRP/regenerative injections. When appropriate, we use:
- Intra‑articular corticosteroid: Short‑term relief of inflammatory flares or advanced OA; ultrasound guidance where needed; limits on frequency to protect cartilage and systemic health.
- Hyaluronic acid (viscosupplementation): For knee OA in select patients to improve lubrication and cushioning.
- Peri‑tendinous/soft‑tissue steroid: For bursitis or tenosynovitis after ruling out infection/rupture risk.
Injections are adjuncts—not stand‑alone cures—and are integrated into your overall management plan.

Bracing & Orthotics
Correctly chosen support devices reduce pain and improve function.
- Knee unloader braces: For unicompartmental knee OA to off‑load the painful side.
- Wrist/thumb splints: For painful hand OA, De Quervain’s, or CMC arthritis during flares or activity.
- Foot orthoses: For alignment, shock absorption, and plantar support.
We provide custom bracing/orthotics when indicated and align device use with your treatment goals.

Joint Preservation & Surgery
When symptoms persist despite best non‑surgical care, we discuss procedures matched to your diagnosis and goals:
- Joint preservation osteotomies: High tibial osteotomy (HTO), distal femoral osteotomy (DFO), tibial tubercle osteotomy (TTO), and hip‑preserving options in select cases to realign load and protect joint surfaces.
- Arthroscopy: For mechanical symptoms (loose bodies, meniscal tears, focal chondral lesions) in the right context.
- Joint replacement: Total knee, total hip, shoulder replacement—including partial hip and robotic‑assisted options—when arthritis is advanced. See our pages on TKR, THR, and Shoulder Replacement.
We present realistic benefits, risks, timelines, and expected recovery so you can decide with confidence.
Flare Management
Flares are surges of pain, stiffness, or swelling. We help you recognize triggers and manage them safely:
- RA/psoriatic arthritis: Short‑term anti‑inflammatories, adjust DMARDs if needed, and review triggers (infection, missed doses).
- Gout: Early colchicine/NSAID strategy, hydration, and follow‑up for long‑term urate control.
- OA flares: Activity modification, icing/heat, topical NSAIDs, and short courses of oral anti‑inflammatories if appropriate.
If a joint is red‑hot with fever or you cannot bear weight, call us immediately—rule out infection before any steroid use.

Special Situations
Diabetes & hypertension
NSAIDs, steroids, and some DMARDs can affect sugars or BP. We plan medicines and monitoring accordingly.
Infection & vaccination
Screening for TB/hepatitis prior to biologics; vaccine planning (e.g., flu, pneumococcal) while on immunomodulators.
Pregnancy & lactation
Disease control with pregnancy‑compatible medicines; coordinate with obstetrics for safe plans.
Seniors
Fall‑reduction strategies, bone health checks (DXA) where appropriate, and simplified medicine regimens.
Monitoring & Safety
- Follow‑up cadence: Every 4–12 weeks in active disease; 3–6 months when stable.
- Scores & function: Pain, stiffness, swelling counts; DAS28 or RAPID‑3 for RA; patient‑reported function.
- Lab monitoring: CBC, liver/kidney function, lipids (JAK inhibitors), and uric acid for gout control.
- Imaging when needed: Ultrasound/MRI for uncertain inflammation or to guide procedures.
Your plan evolves with your progress. We aim for controlled inflammation, fewer flares, and better daily function.

Cost & Insurance
Costs depend on evaluation (labs/imaging), medicines (DMARDs, biologics, JAK inhibitors), and any injections or procedures. Biologics and viscosupplementation vary widely by brand and coverage. We verify benefits and provide a transparent estimate before scheduling your Arthritis & Rheumatology Care in Delhi.
- Insurance pre‑authorization & benefits check
- Clear estimate of out‑of‑pocket costs
- Cashless/financing options where applicable

How to Prepare
Bring records
Prior clinic notes, lab results, X‑rays/MRI reports, medication list, and allergies.
Medication timing
Know your current doses and last injection dates; note any side effects.
Vaccination history
Useful if starting immunomodulators; we can plan updates if needed.
Lifestyle & goals
Note triggers, work demands, and activity goals (e.g., sit cross‑legged, walk 5 km, return to sport).
Physio preference
We do not provide in‑house physiotherapy. Share your physiotherapist’s details so we can coordinate written protocols.
Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91‑9810117204 to confirm.
FAQs
What’s the difference between osteoarthritis and rheumatoid arthritis?
Can arthritis be cured?
Are injections safe?
Do you provide physiotherapy?
When should I consider surgery?
How long do DMARDs/biologics take to work?
What diet helps gout?
Ready for a clear plan to control pain and protect your joints?
Book an appointment. We’ll confirm your diagnosis and build a plan tailored to your goals.
