Bone Tumor Surgery in Delhi (Limb-Salvage & Reconstruction)
Bone Tumor Surgery in Delhi with Dr. Neelabh focuses on accurate diagnosis, oncologic resection with safe margins, and functional reconstruction—often with limb-salvage techniques. We coordinate closely with medical and radiation oncology and provide a clear, phase-based recovery protocol for your physiotherapist. We do not provide in-house physiotherapy.
Oncologic margins • Limb salvage • Endoprosthesis/biologic options • Multidisciplinary care
Oncologic precision
Careful staging, planned biopsy, and resection with appropriate margins.
Limb-salvage first
Modern reconstructions restore alignment, stability, and function.
Advanced tools
Patient-specific guides, 3D planning, modular tumor endoprostheses.
External physiotherapy
Written rehab protocols; we coordinate with your chosen physiotherapist.
What is Bone Tumor Surgery?
Bone tumor surgery removes abnormal bone growths and, when needed, reconstructs the limb. The surgical plan depends on tumor type (benign, aggressive benign, malignant), location (e.g., around the knee, hip, shoulder), size, and whether it has spread. For malignant tumors and certain benign aggressive lesions, the goal is to achieve oncologic control—removing the tumor with safe margins—while preserving function through limb-salvage reconstruction whenever feasible.
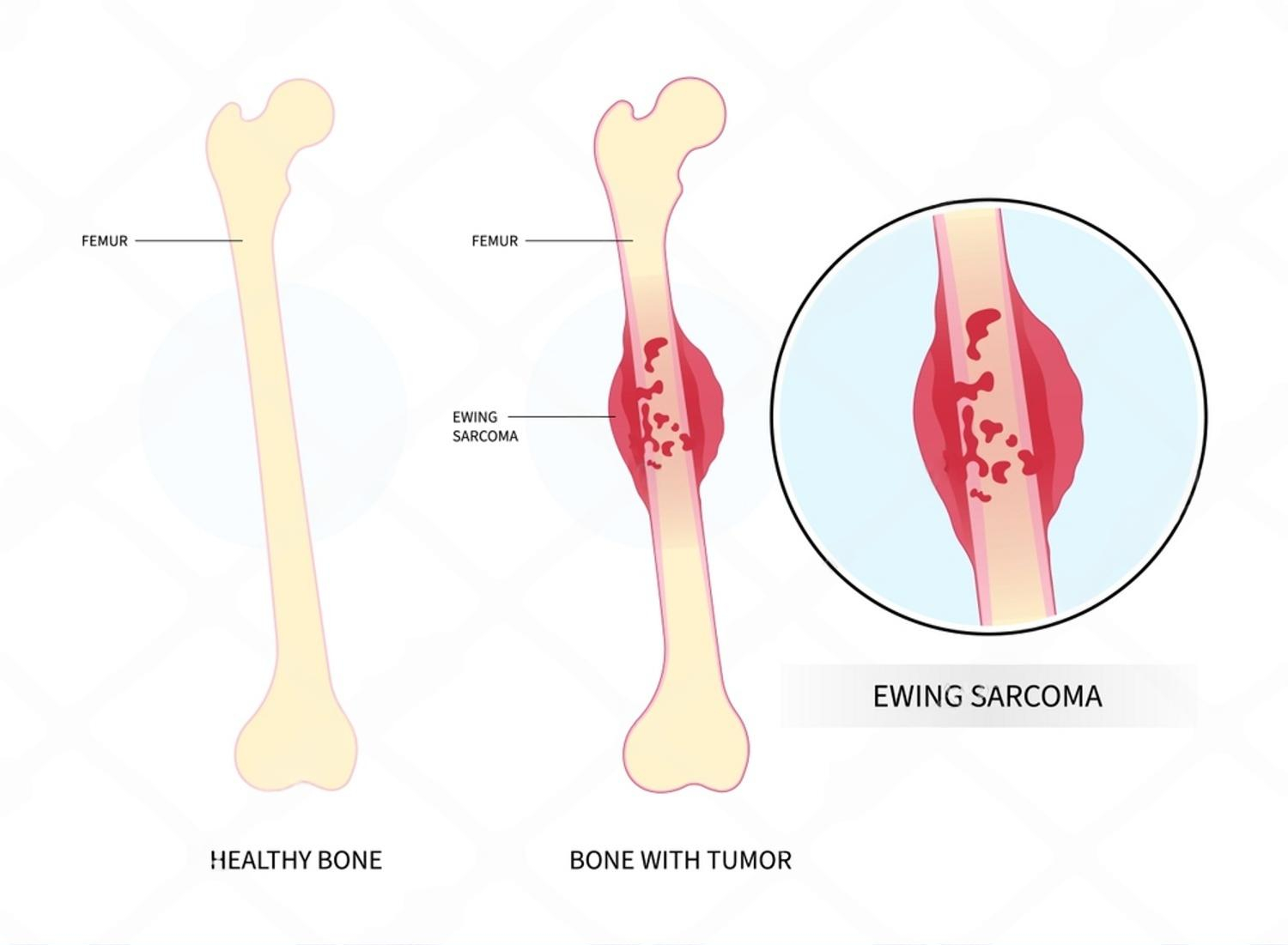
A multidisciplinary approach is essential. Many malignant bone tumors (like osteosarcoma and Ewing sarcoma) require chemotherapy and/or radiotherapy along with surgery. We coordinate with oncology specialists and base decisions on staging, response to therapy, and your individual goals.

Types of Bone Tumors
Benign
Osteochondroma, enchondroma, non-ossifying fibroma—often observed or treated with curettage if symptomatic.
Benign aggressive
Giant cell tumor (GCT), aneurysmal bone cyst (ABC)—treated with extended curettage and adjuvants or resection when needed.
Malignant (primary)
Osteosarcoma, Ewing sarcoma, chondrosarcoma—require staging, oncologic resection, and systemic therapy as indicated.
Metastatic
Cancer spread to bone (e.g., breast, prostate, lung, kidney, thyroid) causing pain or fracture risk—managed with fixation/reconstruction and systemic therapy coordination.
Not all bone tumors are cancer. Careful evaluation avoids over- or under-treatment.
Evaluation & Diagnosis
- Imaging: X-rays for bone architecture; MRI with contrast for local extent and skip lesions; CT for bone detail; CT chest for metastatic survey; PET-CT or bone scan in selected cases.
- Biopsy planning: Core needle/incisional biopsy performed by the surgical team that will perform definitive surgery, with the tract planned along prospective incision lines to avoid contaminating compartments. Unplanned procedures complicate limb salvage.
- Staging: AJCC/Enneking system—assesses grade, site, and spread; guides margins and reconstruction.
- Multidisciplinary review: Tumor board input (orthopaedic oncology, medical oncology, radiology, pathology, radiation oncology) for a unified plan.
If you’ve been advised to “just remove it,” seek an ortho-oncology opinion first—biopsy technique and incision placement can determine whether limb salvage is possible.

Treatment Options
Observation
For small, asymptomatic benign lesions with low fracture risk; periodic imaging confirms stability.
Curettage & adjuvants
For benign aggressive tumors (e.g., GCT, ABC). Extended curettage with local adjuvants (phenol, liquid nitrogen, argon beam) plus cement/plate augments strength.
Wide resection
For malignant or recurrent/aggressive lesions. Goal: remove tumor with an appropriate margin to reduce recurrence.
Systemic therapy
Chemotherapy (e.g., osteosarcoma, Ewing) and targeted agents coordinated with oncology; radiotherapy for specific cases.
Prophylactic fixation
For impending pathologic fractures (e.g., Mirels score), preventing catastrophic breaks and aiding pain relief.
Palliative goals
When cure isn’t feasible, surgery can stabilize bone, reduce pain, and improve function.
Your plan balances oncologic safety with function—decided after full staging and tumor board review.
Reconstruction & Limb-Salvage Techniques
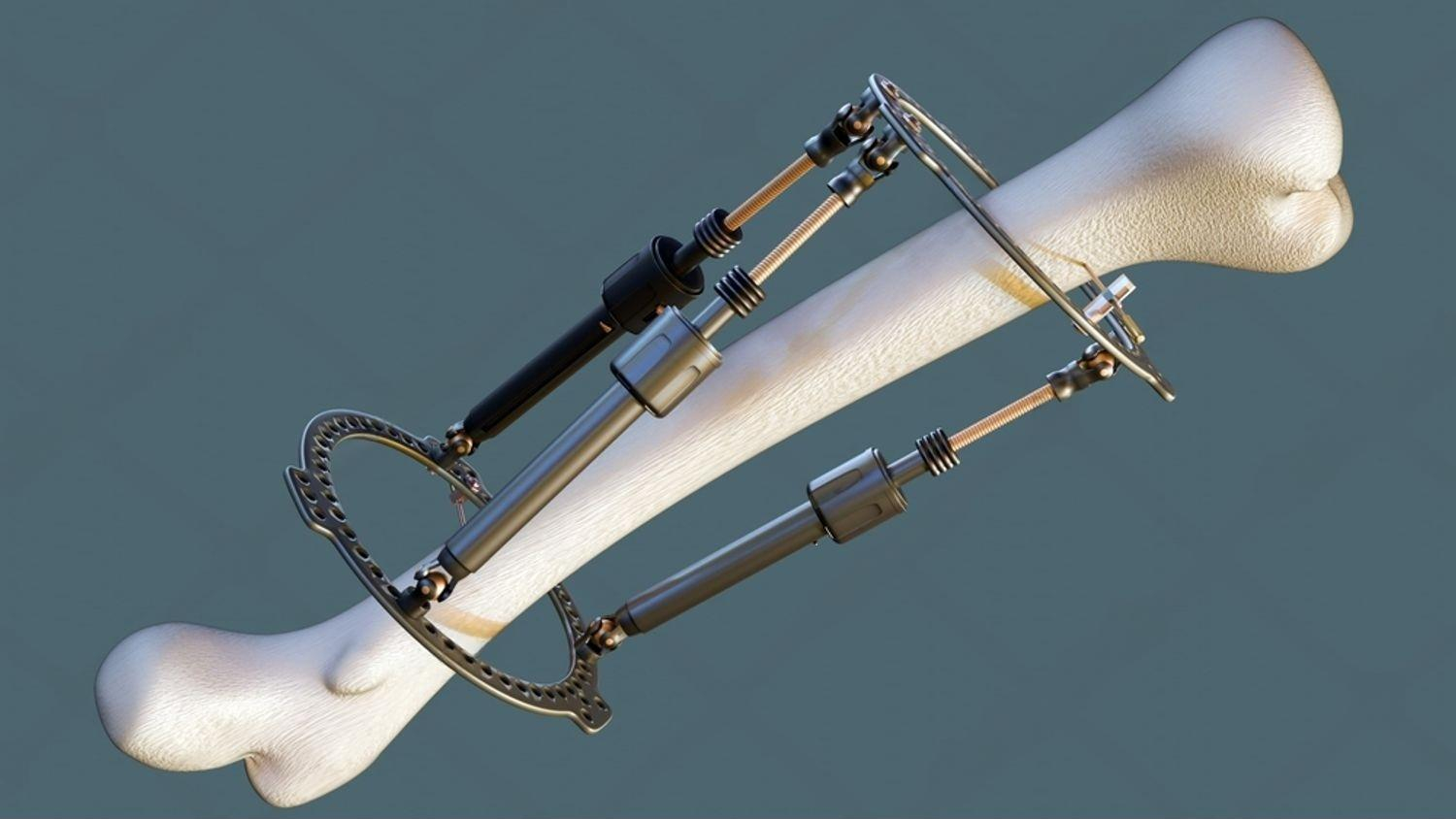
- Tumor endoprosthesis: Modular or custom implants for proximal/distal femur, proximal tibia, proximal humerus; allows immediate stability and early mobilization.
- Biologic reconstruction: Allograft, autograft, allograft–prosthesis composite (APC), vascularized fibula for intercalary defects.
- Intercalary plating/nailing: For diaphyseal resections preserving adjacent joints.
- Expandable implants: In skeletally immature patients to address limb length with growth.
- Patient-specific planning: 3D planning, cutting guides, and navigation to optimize margins and fit.
Technique choice depends on tumor site, soft-tissue involvement, neurovascular status, and expected durability for your activity level.

Metastatic Bone Disease
Cancer that has spread to bone can cause severe pain and fracture risk. The goals are stability, function, and pain relief—coordinated with systemic therapy. Decisions factor in primary tumor type, expected response to therapy, and overall health.
- Impending fracture: Prophylactic nailing or plating with cement augmentation can prevent breakage and reduce pain.
- Peritrochanteric/proximal femur: Hemi/total hip replacement or IM nailing based on bone loss and joint involvement.
- Spine lesions: Managed with the spine team (decompression, stabilization, vertebroplasty/kyphoplasty) as appropriate.
We coordinate with medical oncology and radiation oncology for comprehensive care.
How Bone Tumor Surgery is Performed
- Anaesthesia & planning: General/regionals as appropriate; imaging and margins reviewed with the team.
- Biopsy tract management: The prior biopsy tract is excised en bloc with the tumor to avoid seeding.
- Oncologic resection: Tumor removed with planned margins (intralesional, marginal, wide) per indication.
- Reconstruction: Endoprosthesis, plating/nailing with graft, or biological solutions restore stability and limb length.
- Closure & pathway: Wound closure, drains when needed, DVT prevention; recovery milestones documented.
Margin choice is guided by tumor biology and location; the aim is oncologic safety with maximal function.
Recovery & Follow-up
- Day 0–2: Pain control, limb elevation, protected mobilization as per reconstruction.
- Week 1–3: Wound checks; progressive walking aids/brace as indicated; gentle range-of-motion where safe.
- Week 4–8: Strength and balance improve; advance weight-bearing per fixation stability.
- Month 3–12: Functional training; surveillance imaging for recurrence and implant integrity.
We do not provide in-house physiotherapy. You’ll receive a written rehab protocol and we coordinate with your chosen physiotherapist (external referrals available).

Cost & Insurance
Costs vary by tumor type, location, imaging, biopsy, need for chemotherapy or radiotherapy, reconstruction choice (endoprosthesis vs biological), hospital stay, and rehabilitation requirements. We verify benefits and provide a transparent estimate before scheduling your Bone Tumor Surgery in Delhi.
- Insurance pre-authorization & benefits check
- Clear estimate of out-of-pocket costs
- Cashless/financing options where applicable

How to Prepare
Medical clearance
Pre-op evaluation, labs, ECG; ensure staging scans and biopsy reports are available.
Medication review
Guidance on blood thinners/diabetes meds; optimize nutrition and haemoglobin.
Oncology coordination
Plan chemotherapy/radiotherapy sequencing with the oncology team.
Home setup
Arrange support, prepare a safe path at home, set up braces/walker if needed.
Informed choices
Discuss reconstruction pros/cons (implant vs biological), expected function, and follow-up surveillance.
Where to Consult Dr. Neelabh
BLK Hospital
A-4-6, Pusa Rd, Near Rajendra Place Metro Station, New Delhi-110005
🕓 4:00 PM – 6:00 PM
Timings may vary—please call +91-9810117204 to confirm.
Frequently Asked Questions
Is every bone tumor cancer?
Can limb-salvage replace amputation?
Who should do the biopsy?
Will I need chemotherapy or radiotherapy?
How long until I can walk?
Do you provide physiotherapy?
Need an expert opinion on a bone tumor?
Let’s plan safe tumor control and the best possible function for your limb.
